If a CPAP machine feels like your only choice for sleep apnea, I want you to know there are other paths forward. While CPAP is often called the "gold standard," it's far from the only solution. For many people, it's simply not the right one.
You can absolutely address the root causes of airway obstruction—and fix sleep apnea without CPAP—through practical, proven strategies like custom-fit oral appliances, targeted muscle exercises, and simple but powerful lifestyle adjustments.
Your Path to Better Sleep Beyond the CPAP Machine
The journey to resolving sleep apnea without a CPAP machine is about much more than just ditching a mask. It’s about finding an integrated approach that restores your health and finally lets you reclaim your nights.
If you're frustrated with CPAP, you're not alone. The reality is that nearly 50% of patients stop using their machine within the first year because of discomfort, noise, or feeling claustrophobic. This isn't a failure on their part; it's a clear sign that we need better, more sustainable alternatives.
This guide is designed to give you the knowledge you need to have informed, confident conversations with your specialist. We'll walk through effective, evidence-based strategies that empower you to find a comfortable treatment that actually fits your life.
Understanding Your Options
Finding the right alternative comes down to your specific situation: the severity of your sleep apnea, your unique anatomy, and your lifestyle. What works wonders for one person might not be the right fit for another, which is why a personalized game plan is so critical.
The main non-CPAP treatment categories we'll explore include:
- Lifestyle and Positional Strategies: These are the foundational changes that often bring significant relief, especially in mild to moderate cases.
- Oral Appliance Therapy: A leading CPAP alternative that uses a custom-fit device, similar to a mouthguard, to keep your airway open while you sleep.
- Myofunctional and Breathing Therapy: Think of it as physical therapy for your airway—specific exercises designed to strengthen airway muscles and promote healthy nasal breathing.
- Advanced Surgical and Implant Therapies: These are targeted solutions for moderate to severe cases where other methods haven't provided the necessary relief.
The most effective sleep apnea treatment is the one you'll actually use, night after night. For so many people, the simplicity and comfort of non-CPAP alternatives lead to better consistency and, ultimately, much better health outcomes.
To give you a clearer picture, I've put together a table that breaks down the most common and effective CPAP alternatives. Think of this as a starting point for a deeper discussion with your healthcare provider.
Comparing CPAP Alternatives At a Glance
This table offers a high-level comparison of common non-CPAP treatments for obstructive sleep apnea, highlighting how they work and who they're best suited for.
| Treatment Approach | How It Works | Best For | Key Benefit |
|---|---|---|---|
| Oral Appliance Therapy | A custom-fit dental device gently moves the lower jaw forward, preventing airway collapse. | Mild to moderate obstructive sleep apnea (OSA). | High patient comfort and adherence; portable and silent. |
| Lifestyle Adjustments | Weight management, positional therapy, and avoiding alcohol reduce physical pressure on the airway. | Mild OSA, or as a complementary therapy for all severity levels. | Improves overall health and can reduce apnea severity. |
| Myofunctional Therapy | Specific exercises strengthen the tongue, soft palate, and throat muscles to prevent collapse. | Individuals with poor oral muscle tone contributing to their OSA. | Addresses a root cause of the obstruction naturally. |
| Hypoglossal Nerve Stimulation | An implanted device stimulates the tongue muscle during sleep to keep the airway open. | Moderate to severe OSA in patients who cannot tolerate CPAP. | A highly effective, long-term solution with no external mask. |
Each of these approaches offers a unique way to manage sleep apnea, moving beyond a one-size-fits-all model and toward a solution that works for you.
Why A Proper Diagnosis Is Your First Step
Trying to fix sleep apnea on your own, without a professional diagnosis, is a bit like navigating a new city without a map. You might stumble upon the right path eventually, but you're far more likely to take wrong turns that waste time and could even be risky. A precise diagnosis isn't just a formality; it's the bedrock of a safe and successful treatment plan.
It's easy to self-diagnose based on snoring or feeling exhausted during the day, but these symptoms don't tell the whole story. They don't reveal the severity of your condition. This is a crucial distinction, because a non-CPAP solution that works wonders for mild apnea could be completely ineffective—or even dangerous—for someone with a severe case.
A formal diagnosis gives us the objective data we need to make informed decisions. It takes you out of the world of guesswork and into a clear, actionable strategy designed for your specific physiology.
Decoding Your Sleep Study Results
The first step is almost always a sleep study, which can be done either in a specialized lab or right in your own bed. The goal is to measure how often you stop breathing during the night and, just as importantly, how much your blood oxygen levels drop.
- Home Sleep Apnea Test (HSAT): This is often the starting point. It's a convenient option where you use a simple, portable monitor to record your breathing, oxygen levels, and heart rate. We've detailed how to diagnose sleep apnea at home so you can see if it’s a good fit for you.
- In-Lab Polysomnogram (PSG): For more complex situations or when an HSAT isn't conclusive, this is the gold standard. It's a more comprehensive overnight study at a sleep center that tracks brain waves, eye movements, and muscle activity, giving a complete picture of your sleep.
No matter which test you have, the most important number you'll get is your Apnea-Hypopnea Index (AHI). This figure represents the average number of times per hour you experience an apnea (a complete stop in breathing) or a hypopnea (a partial blockage).
Your AHI score isn't just a number; it's the key that unlocks the right treatment path. It classifies your condition, telling your specialist which therapies have the highest probability of success for you.
What Your AHI Score Really Means
Understanding your AHI is absolutely essential if you're looking for ways to treat sleep apnea without CPAP. This score categorizes the severity of your condition, and that severity level directly points to the most appropriate alternatives.
- Mild Sleep Apnea (AHI 5-15): You’re having 5 to 15 breathing events an hour. For people in this range, lifestyle changes, positional therapy, and custom-fit oral appliances are often highly effective first-line treatments.
- Moderate Sleep Apnea (AHI 15-30): With 15 to 30 events per hour, the condition requires a more robust intervention. A custom oral appliance is a leading choice here, but a thorough evaluation of your airway is critical to make sure it's the right solution.
- Severe Sleep Apnea (AHI >30): Experiencing more than 30 breathing interruptions every hour puts significant strain on your heart and entire body. CPAP is often the primary recommendation, but if you can't tolerate it, alternatives like hypoglossal nerve stimulation or other advanced therapies can be explored.
This chart helps visualize how a proper diagnosis guides your treatment, leading to CPAP or effective alternatives like a custom oral appliance.
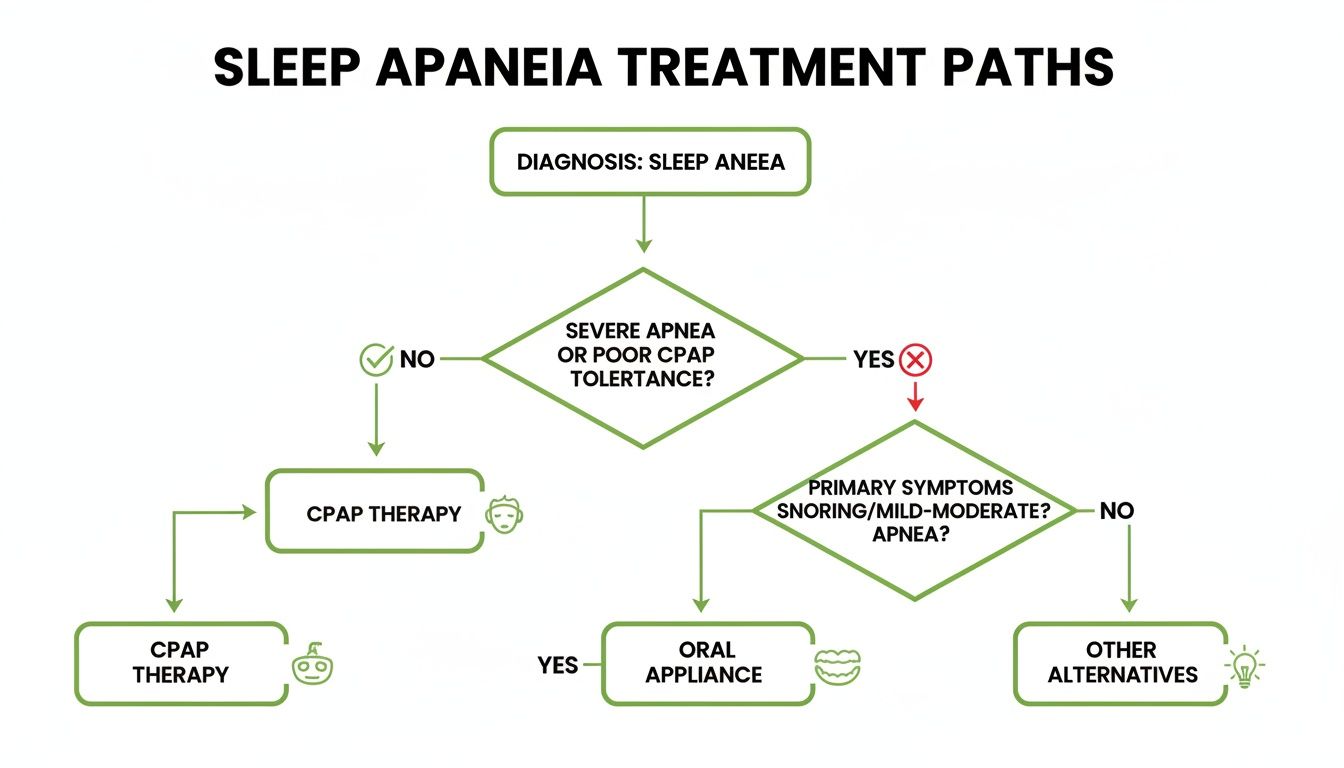
As you can see, the path to feeling better starts with a diagnosis, which then branches out into different solutions based on your specific needs.
But it’s not just about the numbers. A truly comprehensive evaluation also involves a specialist examining your unique airway anatomy. Things like a narrow palate, enlarged tonsils, or a recessed jaw could be the physical root cause of the obstruction. Identifying these factors is key to choosing a treatment that fixes the source of the problem, not just the symptoms.
Foundational Changes for Better Breathing

Before we get into specific therapies and devices, it’s critical to start with the basics. For a lot of people, especially those with mild to moderate sleep apnea, simple lifestyle adjustments aren't just an afterthought—they can be the most powerful treatment of all.
These strategies are all about addressing the root factors that cause your airway to collapse in the first place. Think of them as the essential building blocks for any non-CPAP plan. By focusing on things you can control, like your weight, sleep position, and evening routine, you create a solid foundation for breathing better all night long.
The Connection Between Weight and Your Airway
Excess body weight is hands-down one of the biggest risk factors for obstructive sleep apnea, and the reason is purely anatomical. When you gain weight, fat can accumulate in the soft tissues of the neck and throat.
This added tissue physically narrows your airway, making it much more likely to collapse when your muscles relax during sleep. It's amazing how even a modest amount of weight loss can free up a surprising amount of space in your airway.
In fact, research shows that losing just 10% of your body weight can slash your AHI score. It's often the single most effective first step you can take. Beyond just breathing, studies have shown that even small amounts of weight loss deliver cardiovascular benefits, like improvements in blood pressure, that are comparable to what you'd get with CPAP therapy.
Making Your Sleep Position Work for You
Your sleeping position has a huge impact on whether your airway stays open or not. When you sleep flat on your back, gravity becomes your enemy. It allows your tongue and soft palate to fall backward, blocking your airway and triggering an apnea event.
For many people, their AHI is dramatically higher when they sleep on their back versus their side. This is called positional sleep apnea, and the fix can be surprisingly simple: positional therapy.
Pro Tip: A classic "tennis ball trick" is a great way to start. Just sew a pocket onto the back of an old t-shirt and pop a tennis ball in. If you roll onto your back, the discomfort will naturally train you to shift back to your side.
If you're looking for a more modern approach, there are some great tools available:
- Specialized pillows: Body pillows and contoured cervical pillows are designed to make side-sleeping more comfortable and sustainable all night.
- Wearable devices: These small gadgets are worn on your chest or neck. They vibrate gently when you roll onto your back, prompting you to change position without fully waking you up.
This one change can be an absolute game-changer, especially if your apnea is mild and mostly happens when you're on your back.
Why Evening Habits Matter So Much
What you do in the hours before bed can either set you up for success or completely sabotage your efforts. Alcohol and certain medications—like sedatives or muscle relaxers—are particularly problematic for anyone with sleep apnea.
These substances depress your central nervous system, causing all the muscles in your body to relax. That includes the critical muscles in your throat that work to keep your airway open while you sleep.
When those muscles get too relaxed, your airway is far more likely to collapse. That evening drink might make you feel sleepy, but it almost always worsens snoring and increases both the frequency and length of apnea events. For anyone serious about managing sleep apnea without a CPAP, avoiding alcohol and sedatives within three to four hours of bedtime is non-negotiable. For more ideas, you can check out our guide on how to improve sleep quality naturally.
Oral Appliance Therapy: A Comfortable and Effective CPAP Alternative

For a lot of people dealing with mild to moderate sleep apnea, the idea of CPAP is a non-starter. This is where Oral Appliance Therapy (OAT) comes in. It’s a powerful and liberating alternative that’s not just effective but fits seamlessly into your life without the noise and hassle of a machine.
First, let's be clear: when we talk about an "oral appliance," we are not talking about the boil-and-bite mouthguards you find at a drugstore. Those aren't designed or approved for a medical condition like sleep apnea. We're talking about a sophisticated, custom-fit medical device called a Mandibular Advancement Device (MAD).
These devices are prescribed by a sleep physician and then meticulously crafted by a dental sleep medicine specialist. They look a bit like a sleek, clear retainer, but their function is incredibly precise. The device gently shifts your lower jaw and tongue slightly forward while you sleep, just enough to keep your airway from collapsing and triggering an apnea event.
The Custom-Fit Advantage
The whole process starts with a detailed look at your unique oral anatomy. A specialist will use advanced digital scanners to create a perfect 3D model of your teeth and jaw—no messy, gag-inducing impression trays required.
This digital blueprint is used to create an appliance that fits your mouth and your mouth alone, which is key for both comfort and clinical success. Once your device is ready, the specialist works with you through a careful calibration period, making tiny adjustments to find that "sweet spot" where your apnea is resolved without causing any jaw discomfort.
One of the biggest wins for oral appliances is that people actually use them. Because they're small, silent, and easy to travel with, patient compliance is so much higher than with CPAP. A treatment, after all, only works if you stick with it.
A landmark 10-year follow-up study showed that 86% of patients using oral appliances kept up with their treatment and maintained successful results over the entire decade. That high success rate comes down to consistency.
Long-Term Success and Patient Satisfaction
When you look at long-term outcomes, oral appliances really hold their own. While CPAP is incredibly effective when used, research has found that patients with oral appliances use their therapy for an average of 2.5 hours longer per night compared to CPAP users. All those extra hours add up to better health and feeling truly restored in the morning.
The real-world benefits become obvious when you hear what patients love about them:
- Silence: There's no motor, no pump, and no hissing air. Your bedroom stays quiet for you and your partner.
- Portability: The device fits in a small case you can slide into a pocket or carry-on. It makes travel for work or vacation simple.
- Freedom of Movement: You can sleep in any position you want without worrying about tangled hoses or a mask shifting out of place.
- No Dryness or Irritation: You can say goodbye to the dry mouth, sinus congestion, and red marks on your face that often come with a CPAP mask.
These quality-of-life improvements are a huge reason why so many people looking to fix sleep apnea without CPAP find lasting success with oral appliance therapy. It feels less like a medical intervention and more like a simple part of your nightly routine. And for those who want to take their treatment a step further, combining OAT with exercises can be a great strategy. You can learn more in our guide on myofunctional therapy for sleep apnea.
Exploring Advanced Treatment Options
When lifestyle changes and oral appliances haven't delivered the results you need, it's easy to feel stuck—especially if you have moderate to severe sleep apnea. But this is often the point where some of the most targeted and effective treatments come into the picture, offering real hope for finally getting a good night's sleep.
These advanced therapies are for specific situations, like when a physical (or anatomical) issue is the main cause of airway obstruction or when someone simply can't tolerate CPAP. They represent a significant step up from foundational strategies, providing powerful solutions that get to the root of the problem.
Just know that these options almost always involve a thorough evaluation with an Ear, Nose, and Throat (ENT) specialist or an oral surgeon to see if you're a good candidate. They aren't a first-line defense, but they're a crucial part of the toolkit for those who need a different path forward.
Hypoglossal Nerve Stimulation: An Implantable Solution
One of the most promising advancements in sleep medicine is Hypoglossal Nerve Stimulation (HNS), probably best known by the brand name Inspire. Think of it as a pacemaker, but for your tongue. It’s a small device implanted under the skin that works from the inside to keep your airway open while you sleep—no mask, no hose.
The system is placed during a minimally invasive outpatient procedure. At night, you just turn it on with a small remote. As you breathe, the device sends gentle, precisely timed pulses to the hypoglossal nerve, which controls your tongue's movement. This stimulation nudges the tongue forward just enough to keep it from falling back and blocking your airway.
For many people who have struggled with CPAP, this therapy is a game-changer. As the surgical techniques and device programming have improved, success rates have climbed. We're now seeing high patient adherence and consistent, long-term improvements for up to five years, with success rates hitting 75-80%. You can learn how the technology has evolved and see the data for yourself.
HNS is specifically for people with moderate to severe obstructive sleep apnea who can't get consistent benefit from CPAP. Before the procedure, a drug-induced sleep endoscopy (DISE) is often done to make sure the patient's airway collapse pattern is one that will respond well to stimulation.
When Surgical Intervention Is the Right Path
Sometimes, the cause of sleep apnea is a specific, correctable anatomical problem in the airway. For those people, a targeted surgery can offer a permanent fix by physically creating more space for air to flow. And while surgery is always a big decision, modern procedures are far more precise and less invasive than they used to be.
An ENT or maxillofacial surgeon can pinpoint exactly where the obstruction is happening and recommend a procedure to fix it.
Common surgical options include:
- Uvulopalatopharyngoplasty (UPPP): This procedure trims excess tissue from the soft palate and uvula to widen the airway at the back of the throat. It's often a good option for people with large tonsils or a long, floppy soft palate.
- Maxillomandibular Advancement (MMA): A more involved but highly effective surgery that moves both the upper and lower jaws forward. This one move dramatically enlarges the entire airway, from behind the tongue to the soft palate, making it a powerful solution for severe cases.
- Nasal Surgery: Occasionally, the blockage isn't in the throat but in the nose. Procedures like a septoplasty (to straighten a deviated septum) or turbinate reduction can open up the nasal passages, which can significantly reduce the severity of sleep apnea events.
Choosing an advanced therapy is a decision you'll make together with your sleep medicine team. It’s all about finding a comfortable, long-term way to fix sleep apnea without CPAP so you can get the safe, restorative sleep your body needs to thrive.
Your Questions, Answered
As you start looking into how to treat sleep apnea without a CPAP, it's completely normal to have a lot of questions. It’s a big step, and you want to be sure you're making the right choice for your health. Let's tackle some of the most common things we hear from patients who are exploring their options.
This isn't about finding a single magic bullet. It's about getting you the clear, honest information you need to make a confident decision with your sleep specialist. Understanding the details of each approach is the key to finding something that not only works but that you can actually live with long-term.
Can I Really Fix My Sleep Apnea Completely Without CPAP?
This is the big question for so many people, and for some, the answer is yes—it’s absolutely possible. For individuals with mild OSA that's tied to things like excess weight or poor muscle tone in the airway, it is sometimes possible to fully resolve the condition. This usually involves a commitment to significant, sustained weight loss combined with dedicated myofunctional therapy to retrain the muscles around your airway.
But for most people, especially those with moderate to severe OSA or specific anatomical issues, "fixing" it really means managing it effectively with a long-term solution. The goal is to get rid of the health risks and give you your quality of life back with a treatment you can use comfortably every night, like a custom oral appliance. The only way to know what’s realistic for you is to get a full evaluation with a specialist.
We should really reframe the word "fix" as "successful long-term management." For many, an oral appliance or another non-CPAP therapy becomes a lifelong tool for healthy sleep, much like glasses are for clear vision. It successfully manages the condition, letting you live free of symptoms and health risks.
Are Over-the-Counter Mouthguards the Same as Custom Oral Appliances?
Not even close. This is a critical point for both your safety and your treatment's effectiveness. It's so tempting to grab a quick, cheap "boil-and-bite" guard you see online or at a pharmacy, but this is one area where you absolutely cannot cut corners.
Over-the-counter mouthguards are not approved by the FDA for treating sleep apnea, and for good reason. Here’s why they’re a poor—and risky—choice:
- They aren't adjustable: A custom oral appliance is a Class II medical device. A trained clinician can fine-tune it with millimeter precision to find the exact jaw position that keeps your airway open. OTC guards are static; you can't adjust them.
- They can cause real harm: A poorly fitting device can lead to serious jaw problems (TMD), shift your teeth in unwanted ways, or permanently misalign your bite over time.
- They're often ineffective: Without the ability to calibrate the device, you have no way of knowing if it’s actually keeping your airway open or stopping your apnea events.
Trying to treat a serious medical condition like sleep apnea with an OTC device is a gamble with your health. A custom appliance, on the other hand, is a safe, prescribed medical treatment designed specifically for your unique anatomy.
How Do I Know Which Non-CPAP Option Is Right for Me?
The right treatment is deeply personal. It depends on a handful of key factors, and there is no single "best" alternative—only the best alternative for you. Finding that fit requires a collaborative approach led by an expert.
Your sleep specialist or a dental sleep medicine expert will walk you through the decision by looking at:
- Your Apnea Severity: Your AHI score is the starting point. Mild cases have a wider range of options, while more severe cases need more powerful interventions.
- Your Airway Anatomy: A physical exam will show whether your obstruction is coming from your tongue, soft palate, jaw position, or even your nasal passages. This points us directly toward the most logical treatment.
- Your Lifestyle and Preferences: Do you travel a lot? Are you a particularly light sleeper? Your daily habits and personal comfort are huge factors for sticking with a treatment long-term.
For example, a patient with moderate apnea caused by a recessed jaw is often a perfect candidate for an oral appliance. On the other hand, someone with severe apnea who just can't tolerate CPAP might be a great fit for hypoglossal nerve stimulation if their airway collapse happens in a specific way.
How Long Does It Take for These Alternative Treatments to Work?
The timeline for seeing results can vary quite a bit based on the treatment you choose. Unlike the instant "on" switch of a CPAP machine, some of these alternatives require an adjustment period or show gradual improvement over time.
- Oral Appliance Therapy: Many patients feel a big difference on the very first night. However, it can take a few weeks—or even a couple of months—of careful, precise adjustments with your specialist to hit that sweet spot of maximum effectiveness and comfort.
- Lifestyle Changes: The benefits of weight loss are gradual but incredibly powerful. As you lose weight, you’ll likely notice a steady reduction in snoring and daytime sleepiness.
- Myofunctional Therapy: Patients often report feeling changes in muscle tone and control within a few weeks of starting their daily exercises. We typically see clinically significant improvements in AHI after 3-6 months of consistent practice.
- Surgical or Implant Therapies: These have a built-in healing and activation period. With hypoglossal nerve stimulation, for instance, the device is usually turned on about a month after the procedure. It’s then fine-tuned over the next few months to achieve the best results.
Patience is key with any non-CPAP approach. Working closely with your provider is the best way to stay on track and get the outcome you're looking for.
At the Pain and Sleep Therapy Center, we specialize in creating personalized, non-CPAP treatment plans that address the root cause of your sleep apnea. If you're ready to explore comfortable and effective alternatives, schedule your consultation today.