Obstructive Sleep Apnea (OSA) is a serious, surprisingly common sleep disorder where your breathing doesn't just get shallow—it completely stops and starts, over and over, all night long.
This isn't just loud snoring. It’s what happens when the muscles in the back of your throat relax a little too much during sleep, causing a physical blockage of your airway. The result is a destructive cycle of suffocation and arousal that completely shatters your sleep quality.
The Nightly Struggle: A Deeper Look
Think of your airway as a flexible straw. While you're awake, your muscles hold it open so air can flow easily. But when you fall asleep, those same muscles—especially in your throat and around your tongue—naturally relax. For someone with OSA, this relaxation goes too far.
The soft tissues collapse, pinching the straw completely shut. Airflow stops. This pause in breathing, called an apnea, can last for 10 seconds or even longer. As you're cut off from oxygen, the O2 levels in your blood start to plummet. Your brain has a powerful survival instinct, and it immediately senses this danger and sounds the alarm.
That alarm is a micro-arousal—a brief, often unconscious jolt that forces you awake just enough to tighten your throat muscles and reopen the airway. This is often followed by a loud gasp, snort, or choking sound as you finally take a breath. You get your oxygen levels back to normal and fall back asleep, usually with no memory of what just happened.
And then the cycle repeats.
The Repetitive Cycle of Disruption
For someone with moderate to severe OSA, this life-or-death cycle can happen 30 or more times every single hour. That can add up to hundreds of these events a night, preventing your brain and body from ever reaching the deep, restorative stages of sleep they desperately need.
You might be in bed for eight hours, but your body isn't resting. It's running a marathon of survival.
This constant interruption is the reason you can wake up feeling completely exhausted after what should have been a full night's sleep. Your body never gets the chance to properly repair and recharge, which leads directly to the profound daytime fatigue, brain fog, and irritability so common with this condition.
The illustration below shows this destructive cycle in three simple steps.
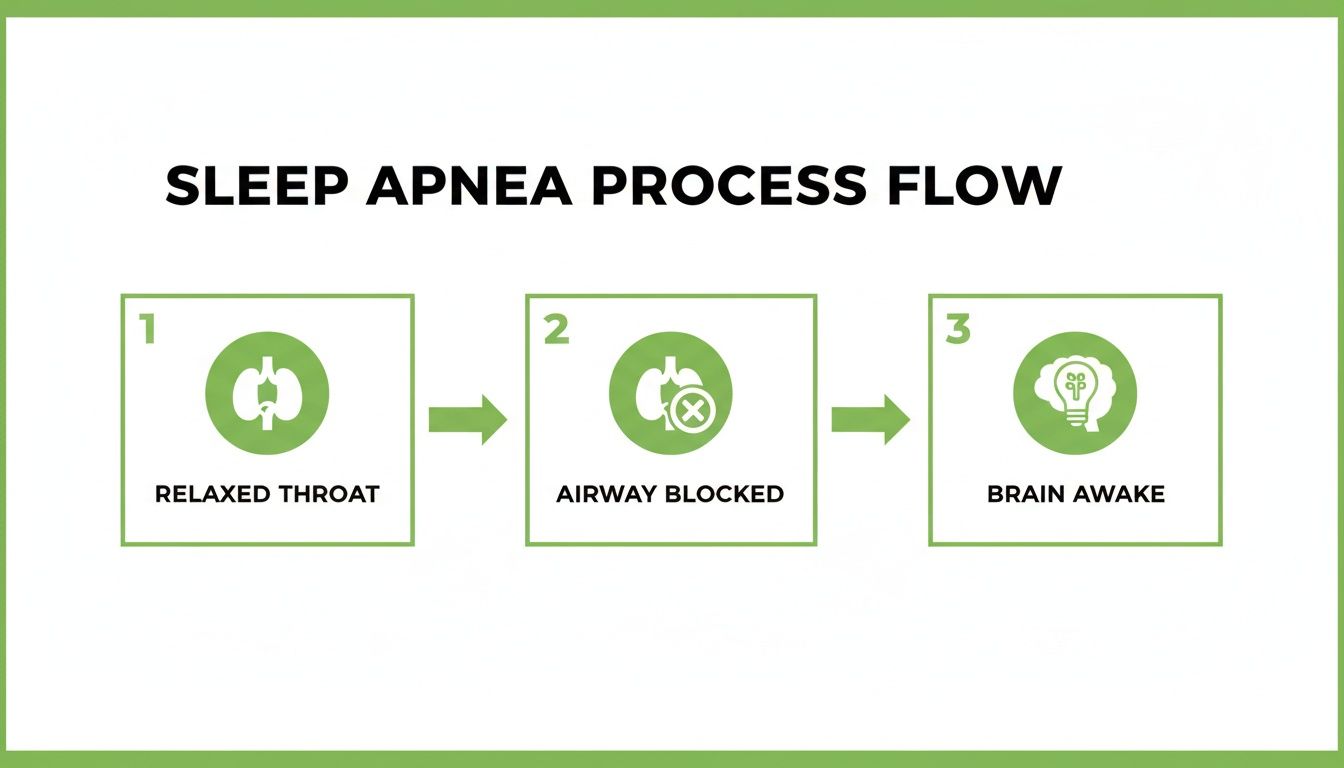
As you can see, it’s a simple but damaging sequence: throat muscles over-relax, the airway becomes blocked, and the brain has to wake you up just to take a breath.
Anatomy of a Sleep Apnea Event
To really grasp what's happening, it helps to break down the rapid sequence of events that puts so much stress on your system.
| Stage | What Happens in Your Body |
|---|---|
| Muscle Relaxation | As you drift off to sleep, the soft tissues at the back of your throat relax too much. |
| Airway Collapse | The relaxed tissue creates a physical blockage, stopping airflow for 10+ seconds. |
| Oxygen Drop | With no air coming in, your blood oxygen levels fall, triggering a panic signal to your brain. |
| Brain Arousal | Your brain briefly wakes you up, tensing the muscles to force the airway open again. |
| Cycle Repeats | You fall back asleep, and the process starts over, destroying healthy sleep all night long. |
This isn't just a minor inconvenience; it's a significant physiological stressor that, night after night, takes a serious toll on your long-term health.
Uncovering the Causes and Risk Factors of OSA
So, why does obstructive sleep apnea affect some people and not others? The answer isn't a single "aha!" moment. Instead, it’s usually a combination of your unique anatomy, daily habits, and even the way you breathe when you're awake.
Getting to the bottom of these root causes is the first real step toward a solution that fixes the problem—not just puts a bandage on the symptoms.
Some risk factors are simply part of your physical makeup. Think of them as the inherited blueprint for your airway.

Anatomical and Genetic Factors
The structure of your face and the size of the soft tissues in your mouth play a huge role in your risk for OSA. These are things you're born with, and they can't be changed with diet or exercise alone.
- A Narrow Jaw or Recessed Chin: A smaller lower jaw can crowd the tongue, pushing it backward toward the throat and shrinking the airway.
- A Large Tongue (Macroglossia): When the tongue is naturally big for the size of the mouth, it's more likely to fall back and block your breathing during sleep.
- Enlarged Tonsils or Adenoids: These are a very common culprit, especially in children, because they can physically obstruct the back of the throat.
- A High-Arched or Narrow Palate: This shape leaves less room in the nasal cavity and mouth for both your tongue and for air to flow freely.
- Deviated Septum: A crooked nasal passage can easily turn you into a "mouth breather"—a habit that directly destabilizes your airway.
These built-in traits create a natural tendency for the airway to collapse. When you add other risk factors into the mix, the likelihood of developing OSA skyrockets.
Lifestyle and Functional Influences
While you can't change your anatomy, you can modify several factors that have a direct impact on your airway. These usually tie back to daily habits and overall health.
Understanding the interplay between your body and your habits is key. OSA is rarely caused by just one thing; it's the result of multiple factors compounding over time, creating the perfect storm for airway collapse.
Excess body weight is one of the biggest contributors. Fat deposits can build up around the neck and throat, physically squeezing the airway. Even a modest amount of weight gain can make OSA symptoms much worse.
Alcohol and sedatives before bed are another trigger. These substances relax the throat muscles more than usual, making the airway floppy and prone to collapse.
Your sleeping position matters, too. Sleeping on your back allows gravity to pull the tongue and soft palate straight back, blocking the airway. Many people notice their symptoms get better just by shifting to their side.
The Critical Role of Oral Function
Perhaps the most overlooked cause of OSA is poor oral function—specifically, chronic mouth breathing and incorrect tongue posture. For your airway to be healthy and stable, you need to breathe through your nose with your tongue resting gently against the roof of your mouth.
When you breathe through your mouth, your tongue has to drop down to let air pass. This low tongue posture makes the surrounding muscles weak over time, and they become much more likely to collapse when you sleep. A restricted tongue, or tongue-tie, can make it physically impossible to achieve the correct posture. You can learn more in our guide on how to check for a tongue-tie.
This connection is exactly why fixing how you breathe and use your oral muscles is so fundamental. It shifts the focus from just propping the airway open at night to restoring its natural strength and function all day long.
The number of people diagnosed with sleep apnea is climbing fast, driven by growing awareness and rising obesity rates. In 2023, there were roughly 25,670 thousand diagnosed OSA cases across seven major markets, and the US accounted for a staggering 54% of them. These numbers are only expected to grow, which highlights just how urgently we need effective, root-cause treatments.
Recognizing the Symptoms and Health Dangers
The effects of obstructive sleep apnea reach far beyond the bedroom, impacting nearly every part of your waking life. Since the most dramatic events happen while you're unconscious, many people have no idea they even have a problem.
Often, it’s a bed partner who first notices the telltale signs of trouble. For others, it’s the persistent daytime struggles that finally push them to find some answers.
Understanding these warning signs is the first step toward reclaiming your health. The symptoms really fall into two different buckets: what happens during the night and the consequences you feel all day long.

Night Vs Day: The Two Faces of OSA Symptoms
It can be tough to connect the dots between nighttime disruptions you don’t remember and the fatigue or irritability you feel the next day. This table breaks down the most common warning signs to help you see the full picture of how OSA affects both your sleep and your waking hours.
| Symptom Category | Common Warning Signs |
|---|---|
| During Sleep | • Loud, disruptive snoring • Pauses in breathing (witnessed apneas) • Gasping or choking for air • Restless tossing and turning • Frequent nighttime urination |
| During the Day | • Overwhelming daytime sleepiness (EDS) • Morning headaches • "Brain fog" or trouble concentrating • Irritability, anxiety, or mood swings • Waking with a dry mouth or sore throat |
Recognizing patterns in both columns is a strong indicator that it's time to investigate further, as these symptoms paint a clear picture of a body struggling for air night after night.
The Daytime Consequences of Poor Sleep
The most devastating impact of OSA is felt during your waking hours. When your body never gets the restorative sleep it needs, the consequences build up, affecting your energy, mood, and even your ability to think clearly.
Excessive Daytime Sleepiness (EDS) is a hallmark symptom, but its severity is often underestimated. It’s not just feeling tired—it’s an overwhelming, persistent state of exhaustion that can make work, driving, and even simple conversations feel like monumental tasks.
Globally, this profound sleepiness affects a staggering 39.9% of people with OSA. The economic toll is immense; in the US alone, workplace and vehicle accidents linked to untreated OSA are estimated to cost $15.9 billion annually and result in approximately 1,400 fatalities. You can review the full data in this American Academy of Sleep Medicine indicator report.
Other critical daytime symptoms include:
- Morning Headaches: Waking up with a dull, throbbing headache is often caused by low oxygen and high carbon dioxide levels in the blood overnight.
- Difficulty Concentrating: "Brain fog" is extremely common, making it hard to focus, remember details, or complete complex tasks.
- Mood Swings and Irritability: Chronic sleep deprivation puts immense stress on your nervous system, leading to a short temper, anxiety, and even depression.
- Dry Mouth or Sore Throat: Waking with a parched throat is a direct result of mouth breathing all night as your body struggles to get enough air.
The Long-Term Health Dangers of Untreated OSA
If left untreated, the repeated drops in oxygen and the stress of constant waking put enormous strain on your entire cardiovascular system. This nightly struggle is directly linked to some of the most serious chronic health conditions.
Untreated obstructive sleep apnea significantly increases your risk for:
- High Blood Pressure (Hypertension): The frequent oxygen drops cause surges in adrenaline, raising your blood pressure and keeping it elevated over time.
- Heart Disease: OSA is a major risk factor for heart attacks, atrial fibrillation (an irregular heartbeat), and heart failure. The strain on the heart is constant.
- Type 2 Diabetes: Sleep deprivation interferes with your body's ability to use insulin properly, increasing the risk of developing insulin resistance and diabetes.
- Stroke: The combination of high blood pressure and reduced oxygen flow to the brain makes a stroke much more likely.
Recognizing these symptoms for what they are—warnings from your body—is crucial. Obstructive sleep apnea is not a personal failing or something to ignore; it is a serious medical condition with life-threatening consequences that demands professional attention.
How Obstructive Sleep Apnea Is Diagnosed
Moving from a suspicion to a real diagnosis of obstructive sleep apnea is a clear, step-by-step process. It starts with recognizing the signs in your daily life and then moves toward a professional evaluation to find out what’s truly happening while you're asleep. Understanding this path is the first step toward taking back control of your health.
The journey often kicks off with a simple self-check. Screening tools like the STOP-BANG questionnaire are widely used because they help you and your doctor quickly get a sense of your risk. It’s a straightforward checklist asking about Snoring, Tiredness, Observed apneas, and high blood Pressure, along with other key factors like BMI, Age, Neck size, and Gender.
But a screening tool isn’t a diagnosis—it's just a signpost. The next real step is a consultation with a specialist who understands the intricate connection between your anatomy and your airway.
The Initial Professional Evaluation
During your first visit, a specialist will do a lot more than just a quick look. They’ll perform a detailed physical examination focused on the very structures that can impact your breathing. It's a careful assessment of your head and neck anatomy.
This evaluation usually includes:
- A deep dive into your medical history and a conversation about your specific symptoms, from snoring to how tired you feel during the day.
- An examination of your jaw structure, checking for things like a recessed chin or narrow dental arches that could be crowding your tongue.
- An assessment of your soft tissues, including the size of your tongue, tonsils, and soft palate.
- An analysis of your bite and oral posture to spot signs of chronic mouth breathing or poor tongue placement.
This comprehensive look helps build a clear picture of what might be obstructing your airway before any definitive tests are ordered.
Demystifying the Sleep Study
The gold standard for diagnosing OSA is a sleep study. This is what measures exactly what happens to your body while you sleep. There are two main types, and the right one for you often depends on your overall health and the complexity of your symptoms.
In-Lab Polysomnogram (PSG): This is the most thorough test, done overnight in a specialized sleep center. A technician monitors you while sensors track everything from brain waves and eye movements to muscle activity, heart rate, breathing patterns, and blood oxygen levels. A PSG provides a massive amount of data, helping doctors not only diagnose OSA but also rule out other complex sleep disorders.
Home Sleep Apnea Test (HSAT): For many, a home sleep test is a much more convenient and equally effective option. You’ll use a portable monitoring device that you wear overnight in your own bed. An HSAT focuses on measuring breathing effort, airflow, and oxygen saturation, which is typically enough information to accurately diagnose most cases of obstructive sleep apnea.
A sleep study isn’t just about getting a "yes" or "no" on sleep apnea. It's about understanding its severity. The data gives us the objective evidence we need to create a treatment plan that’s actually built for you.
Understanding Your AHI Score
After your sleep study, your results will highlight a critical number called the Apnea-Hypopnea Index (AHI). This metric is the key to understanding just how serious your condition is. It tells you the average number of apnea (complete breathing pauses) and hypopnea (partial blockages) you experience per hour of sleep.
Your AHI score is used to classify the severity of your OSA:
- Normal: Fewer than 5 events per hour
- Mild OSA: 5 to 14 events per hour
- Moderate OSA: 15 to 29 events per hour
- Severe OSA: 30 or more events per hour
This number makes the diagnosis tangible. An AHI of 25, for instance, means your body is being jolted out of restful sleep by a breathing disruption roughly every two and a half minutes, all night long. Knowing your AHI is crucial—it quantifies the nightly struggle and helps guide how intensive your treatment needs to be.
Obstructive sleep apnea is a massive global health issue, yet it’s frighteningly underdiagnosed. Globally, an estimated 936 million adults have at least mild OSA, with 425 million dealing with moderate to severe cases. In the United States alone, while about 29.4 million adults are affected, a shocking 80% of these cases—or 23.5 million people—remain undiagnosed. They are left untreated and vulnerable to serious health consequences. You can find more insights in this in-depth indicator report on sleep apnea.
Modern Sleep Apnea Treatments Beyond the CPAP
For decades, the Continuous Positive Airway Pressure (CPAP) machine was the only real game in town for treating obstructive sleep apnea. While it can be a lifesaver, the reality is that many people just can't tolerate the mask, the hose, and the constant forced air. And if a treatment isn't used, it simply doesn't work.
Thankfully, we've moved beyond a one-size-fits-all approach. Modern sleep medicine offers some powerful—and far more comfortable—alternatives that get to the root cause of why the airway collapses in the first place, rather than just propping it open with air. These non-invasive options are opening the door to restful, restorative sleep without the hassle of a traditional CPAP.

Oral Appliance Therapy: A Comfortable Alternative
One of the most effective and popular alternatives to the CPAP is Oral Appliance Therapy (OAT). This approach uses a custom-made device, similar to a sports mouthguard or an orthodontic retainer, that you wear only while you sleep.
It works by gently guiding your lower jaw slightly forward. This small adjustment is all it takes to open up space at the back of your throat, preventing your tongue and soft tissues from collapsing and blocking your airway. Think of it as creating a small, internal scaffold that keeps everything stable all night long.
Oral Appliance Therapy is often a first-line treatment for mild to moderate obstructive sleep apnea. Its comfort and ease of use lead to much higher patient compliance, making it a highly effective solution for many who have struggled with CPAP.
These devices are custom-fitted by a trained dental sleep medicine expert to ensure they're both effective and comfortable. They’re also silent, portable, and easy to care for, which makes them a fantastic choice for anyone looking for a less intrusive treatment.
Orofacial Myofunctional Therapy: Strengthening the Airway
While an oral appliance physically holds the airway open, Orofacial Myofunctional Therapy (OMT) works differently. It’s like physical therapy for the muscles of your tongue, mouth, and throat. The goal isn't just to prop the airway open but to strengthen it so it no longer collapses in the first place.
OMT involves a series of simple, targeted exercises that correct poor muscle habits contributing to OSA. A trained therapist guides you through routines that improve:
- Tongue Posture: Training your tongue to rest naturally against the roof of your mouth, which helps keep the airway open.
- Nasal Breathing: Shifting from mouth breathing to nasal breathing, a critical component of airway stability.
- Swallowing Patterns: Correcting dysfunctional swallowing habits that can weaken throat muscles over time.
By retraining these crucial functions, OMT restores the natural strength and tone of the muscles supporting your airway. This can lead to a significant drop in apnea events and a lasting improvement in your sleep quality. Our clinic provides detailed guidance on myofunctional therapy for sleep apnea as part of our integrated treatment plans.
The Power of Proper Breathing with Buteyko
A close cousin to myofunctional therapy is the Buteyko Breathing Method. This technique is all about restoring healthy, functional breathing patterns. Many people with OSA are chronic over-breathers or mouth-breathers—habits that directly destabilize the airway and disrupt sleep.
The Buteyko method teaches you to breathe calmly and lightly through your nose, both day and night. The exercises help your body become more tolerant of carbon dioxide, which dials down the urge to over-breathe. This results in more stable blood oxygen levels and a calmer nervous system while you sleep.
When you combine the structural support of an oral appliance with the functional retraining from OMT and Buteyko breathing, you're tackling obstructive sleep apnea from every angle. It’s an integrated strategy that moves beyond just managing symptoms to truly address the underlying causes of your condition.
An Integrated Approach to Treating Sleep Apnea
Truly effective sleep apnea treatment is never about just one device or a single quick fix. It’s about creating a complete strategy that addresses your unique anatomy, the way your muscles function, and even your deep-seated breathing habits. We shift the focus away from just managing symptoms and toward restoring proper function to the entire system that keeps your airway open.
This integrated approach always starts with a comprehensive evaluation that looks at the big picture. We don’t just assess your airway; we look at your jaw structure, your tongue posture, and your daily breathing patterns. This foundational knowledge is what allows us to build a truly personalized treatment plan that combines the right tools for your specific needs.
Building a Personalized Treatment Plan
For many of our patients, this plan starts with one comfortable, effective therapy, and we build from there. The goal is to create a multi-layered solution that provides both immediate relief from your sleep apnea and long-term stability for your airway.
- Oral Appliance Therapy (OAT): This is often the cornerstone of treatment. It physically supports the airway while you sleep, providing immediate relief from apnea events.
- Myofunctional Therapy: Think of this as physical therapy for the tongue and throat. We use it to strengthen these muscles, helping them naturally resist collapse on their own.
- Breathing Retraining: Techniques like Buteyko breathing help restore healthy nasal breathing patterns, which are absolutely essential for maintaining a stable airway, both day and night.
This combination ensures you aren't just propping the airway open with a device but actively retraining your body to maintain it independently. It's a proactive method aimed at creating lasting change, not just relying on a machine indefinitely.
Why a Holistic View Is Crucial
This method works because it targets the underlying cause of the airway collapse, not just the symptom. Your jaw, your tongue, and your breathing are all interconnected parts of a single system. By addressing weaknesses in each area, the entire system becomes stronger and more resilient. You can learn more about how targeted exercises contribute to this process in our guide to orofacial myofunctional therapy exercises.
The need for this approach is becoming more critical every year. The prevalence of OSA skyrockets with age; in 2023, the 65+ age group saw approximately 8,870 thousand cases, a massive jump from the 179 thousand in 19-24 year-olds. Severity is also a growing concern, with the US alone having around 6,208 thousand severe cases in 2023. These staggering numbers show why a root-cause approach that offers a lasting solution is more important than ever for reclaiming long-term health and energy. You can explore more data in this report from the American Academy of Sleep Medicine.
Your Questions About Obstructive Sleep Apnea, Answered
As you dig into what obstructive sleep apnea really is, a lot of questions are bound to pop up. It's totally normal. Here are some of the most common ones we hear from patients, with straightforward answers to clear things up and help you feel confident about what to do next.
Can I Have Sleep Apnea if I’m Not Overweight?
Yes, absolutely. While it’s true that extra weight is a major risk factor, we see plenty of patients with OSA who are at a perfectly healthy weight.
The real issue is often anatomy. Things like a recessed jaw, a large tongue, or even enlarged tonsils can create a smaller airway that’s more likely to collapse during sleep, no matter your BMI. This is exactly why a professional airway evaluation is so important—it looks beyond the scale to see what’s really going on.
Is Snoring Always a Sign of Obstructive Sleep Apnea?
Not always, but it’s the #1 red flag. Simple snoring can sometimes just be noise. The kind of snoring that points to OSA, though, is different. It's usually loud and relentless, and you'll hear distinct pauses in breathing followed by a gasp or choking sound as the person struggles for air.
If your snoring is paired with feeling wiped out during the day or any other symptoms, it’s a strong signal that you should get checked out.
For mild to moderate sleep apnea, oral appliances are a proven and highly effective first-line treatment. Their comfort and convenience often lead to better patient compliance compared to other methods.
Are Oral Appliances as Effective as CPAP?
For many people, they are. Oral appliances are an excellent go-to treatment for mild to moderate OSA.
When it comes to severe cases, a CPAP might be the first thing a doctor recommends. But even then, an oral appliance can be a fantastic and effective alternative, especially for anyone who just can't get used to CPAP. The goal is consistent treatment, and the best device is the one you'll actually use every night.
How Long Does It Take for Myofunctional Therapy to Work?
Think of orofacial myofunctional therapy as physical therapy for the muscles around your airway. Many patients start to feel a real difference in their breathing and sleep quality within just a few weeks of doing the daily exercises consistently.
The big, lasting changes—where correct tongue posture and new muscle habits become second nature—typically take a few months to lock in. It’s an investment in retraining your body for better long-term function.
Ready to get to the root cause of your sleep issues and finally get your energy back? The team at Pain and Sleep Therapy Center is here to create a personalized, non-surgical treatment plan that works for you. Schedule your consultation today.