When most people think of temporomandibular joint dysfunction (TMD), the classic symptoms like jaw pain, clicking sounds, and headaches usually come to mind. But this incredibly complex condition often sends out a much wider range of signals—from earaches and facial tension to subtle shifts in your bite. Learning to recognize the full spectrum is the first step toward getting real answers.
Unpacking the Signs of Temporomandibular Joint Dysfunction

That nagging ache you feel just in front of your ear, the tension headache that never seems to go away, or that unsettling "pop" you hear when you yawn—it's easy to write these things off as just stress. But what if they're actually clues pointing to a deeper imbalance? These experiences are often the first whispers of TMD, a condition affecting the intricate hinge system connecting your jaw to your skull.
Think of your temporomandibular joints (TMJ) as the body's most dynamic hinges, working tirelessly so you can talk, chew, and show emotion. When this system gets out of sync—whether from muscle strain, joint inflammation, or structural issues—the ripple effects can be surprisingly widespread. And it’s far more common than many people realize.
In fact, temporomandibular joint dysfunction affects an astonishing 34% of the global population, making it one of the most widespread musculoskeletal disorders out there. Here in the U.S., the National Academies report that somewhere between 11.2 and 12.4 million people live with TMJ-related pain. These numbers highlight just how critical accurate diagnosis and effective care really are. You can dive deeper into the research behind these numbers and learn more about global TMD prevalence from recent studies.
To help you quickly see if what you're experiencing aligns with TMD, we've put together this simple guide.
Quick Guide to Common TMD Symptoms
| Symptom Category | Common Examples |
|---|---|
| Jaw-Specific | Pain, stiffness, clicking, popping, locking, limited movement |
| Head & Face | Headaches (especially in temples), migraines, facial pain, sinus pressure |
| Ear-Related | Earaches, ringing (tinnitus), feeling of fullness or clogging |
| Bite & Teeth | Changes in how teeth fit together, clenching, grinding (bruxism) |
| Neck & Shoulders | Pain, stiffness, tension that radiates from the jaw |
This table is just a starting point. Many patients are surprised to learn how interconnected these symptoms can be.
Why Jaw Pain Is More Than Just a Local Issue
TMD symptoms are rarely contained to just the jaw. Why? Because the TMJ is surrounded by a dense network of muscles, nerves, and ligaments. Any dysfunction here can easily radiate outward, creating a cascade of what seem like unrelated problems.
It’s like a traffic jam on a major highway. A problem in one small area—the joint—can cause backups and disruptions for miles, impacting your head, neck, and even your ears. This is exactly why a stubborn headache might actually be a sign of jaw muscle tension, or why that stuffy feeling in your ear could stem from inflammation in the nearby joint.
Understanding this interconnectedness is key to finding lasting relief. If you only treat the surface-level pain, you often get stuck in a frustrating cycle. A root-cause approach, on the other hand, works to identify and correct the underlying imbalance for a truly sustainable solution.
Key Takeaway: TMD is not just a "jaw problem." It is a complex disorder of the entire jaw system—including the joints, muscles, and surrounding nerves—which explains its incredibly wide array of symptoms.
Recognizing the full pattern of your symptoms is crucial. So many people suffer for years from chronic headaches or facial pain without ever making the connection to their jaw. In the following sections, we’ll break down these symptoms in much more detail, helping you connect the dots between what you're feeling and its potential source so you can take the right next step.
Decoding Jaw Pain, Clicking, and Locking

When people first realize something is off with their jaw, it almost always starts with one of three things: pain, strange noises, or that awful feeling of being stuck. These are the classic calling cards of TMJ dysfunction. Think of them as your body’s alarm system, letting you know the complex machinery of your jaw is no longer running smoothly.
Understanding what these signals mean is the first step toward finding real relief. So, let’s break down what’s actually happening inside your jaw when you experience these common symptoms.
The Many Faces of Jaw Pain
Jaw pain from TMD is rarely a one-size-fits-all problem. It can show up in surprisingly different ways, depending on whether the joint, the muscles, or both are the main source of the trouble.
For some, it’s a dull, persistent ache right in front of the ear—a constant, low-grade throb that seems to get worse as the day goes on. For others, it’s a sharp, stabbing sensation that hits when they chew something tough, yawn too wide, or simply open their mouth. That kind of acute pain often points to an issue inside the joint itself.
Important Distinction: Pain felt directly over the joint can signal inflammation or a mechanical problem with its internal parts. Pain that feels more widespread—in the cheeks, temples, or side of the head—often points to muscle strain and fatigue from overwork.
This pain isn't just a minor inconvenience. It’s a direct message that the joint and its supporting muscles are under serious stress, and ignoring it can allow the underlying problem to get worse.
Understanding Clicks, Pops, and Grinding Sounds
Ever heard a "click" or "pop" when you open your mouth? These sounds are incredibly common and are often one of the first signs of a TMJ issue. Think of your jaw joint like a well-oiled door hinge that opens and closes silently. Now, imagine that hinge is slightly off track—it’s going to creak and pop as it moves.
Your jaw has a small, soft cartilage disc that acts as a cushion between the bones, allowing for that smooth, silent movement.
- Clicking or Popping: This usually happens when that little disc slips slightly out of place as you open your jaw and then snaps back into position. It's like a tiny internal reset button being pushed with every movement.
- Grating or Grinding (Crepitus): This is a much different sound—sandy, gravelly, and rough. It often means the cartilage has started to wear down, causing bone to rub against bone. This is usually a sign of more advanced joint changes, like arthritis.
It’s important to know that not all jaw noises are a crisis. An occasional, painless click might not be anything to worry about. But if that sound comes with pain, limits your movement, or you feel a change in your bite, that’s a clear sign of dysfunction that needs to be checked out.
When Your Jaw Gets Stuck
This is probably the most unsettling symptom of TMD: jaw locking. It’s that terrifying moment when the joint gets stuck, and you can’t fully open or close your mouth. Whether it lasts for a few seconds or much longer, it’s an undeniable sign that you need professional help.
Locking typically happens in two ways:
- Closed Lock: This is when you can’t open your mouth all the way. It’s usually caused by that cartilage disc slipping too far forward and physically blocking the joint from moving—like a doorstop wedged under a door.
- Open Lock: This is less common but more alarming. It happens when you open your mouth too wide (like during a big yawn), and the jaw bone slips past the disc, getting stuck in the open position.
Any kind of jaw locking means the joint's mechanics have significantly failed. It's not something you should try to "pop" back into place on your own. This symptom is a clear signal to consult a specialist who truly understands the complex world of the TMJ.
Unmasking Headaches, Earaches, and Facial Pain
When your jaw is the problem, the pain rarely stays put. For so many of our patients, the most confusing and frustrating symptoms are the ones that show up in seemingly unrelated places, kicking off a long and discouraging search for answers.
The truth is, your jaw doesn't work in a bubble. It's a central hub, deeply connected to a dense network of muscles and nerves that branch out across your entire head, face, and neck. When the jaw joint is overworked or out of balance, the strain creates a domino effect, sending pain signals radiating outward. This is called referred pain, and it’s often the most disruptive symptom of all.
This is exactly why people suffering from chronic headaches or nagging earaches are so surprised when we trace the issue back to their jaw. They’ve often seen specialist after specialist for their head or ear pain, never finding relief because the real source of the problem was missed.
Connecting the Dots to Chronic Headaches
If you struggle with tension-type headaches—that feeling of a tight, squeezing band around your temples, forehead, or the back of your head—your jaw muscles are a likely suspect. One of the main muscles you chew with, the temporalis muscle, is a large, fan-shaped muscle on the side of your head. When it gets overworked from clenching or grinding, it can trigger intense, persistent headaches.
These aren't just minor annoyances; they can be completely debilitating and are frequently mistaken for migraines. Understanding this connection is critical for getting the right diagnosis and, more importantly, the right treatment. You can learn more about this by reading our guide on the hidden link between jaw pain and headaches.
Why Your Ears Are So Affected by Jaw Problems
Have you ever had a deep, dull ache inside your ear that an ENT specialist couldn't explain? Or maybe you deal with a constant ringing (tinnitus) or a feeling of fullness, like your ears are clogged with water. The reason is simple proximity: your temporomandibular joint is located just millimeters away from your ear canal.
When the jaw joint becomes inflamed, the swelling can put direct pressure on the delicate structures of your middle and inner ear. On top of that, the same nerve that controls your jaw muscles also sends branches to your ear. Because of this shared wiring, your brain can easily misinterpret a pain signal from the jaw as coming from the ear.
A Crucial Insight: Ear symptoms without any sign of infection are a classic red flag for TMD. If you've been told your ears look perfectly healthy but they still hurt, feel full, or ring, it’s a strong signal that the problem is coming from your next-door neighbor—the jaw joint.
The Spread of Facial and Neck Pain
The pain doesn't stop at the head and ears. This interconnected network of muscles runs down into your cheeks, neck, and even your upper shoulders. This is why TMD can also trigger symptoms like:
- Sinus-like pain: A feeling of pressure under your eyes or in your cheeks that feels just like a sinus infection.
- Neck stiffness: Chronic tension that limits your range of motion and makes your neck feel tight and sore.
- Shoulder pain: Aching and tightness that seems to come from nowhere but is actually referred pain from overworked jaw and neck muscles.
This kind of widespread facial pain is a hallmark of TMJ dysfunction. In fact, after toothaches, TMD is the second most common cause of orofacial pain, affecting 20-30% of adults to some degree. In the U.S. alone, about 1 in 12 people—roughly 35 million individuals—are living with a TMJ disorder, and studies show that muscle-related (myofascial) pain is a component in 73% of new cases.
Recognizing these referred pain patterns is the first step toward real relief. It validates what you're feeling and shifts the focus from just masking symptoms to fixing the underlying mechanical issue in your jaw.
The Connection Between TMD, Bite, and Sleep
TMD symptoms often sneak up on you in ways that go far beyond simple jaw pain. Two of the most common—and often confusing—are subtle changes to your bite and a serious decline in your quality of sleep.
These two areas are deeply connected. In fact, they often create a frustrating feedback loop where a problem with one makes the other significantly worse. It's a perfect example of how jaw dysfunction can have ripple effects throughout your entire well-being.
When Your Bite Suddenly Feels "Off"
Have you ever woken up feeling like your teeth just don't fit together the way they used to? It’s a strange and unsettling sensation. This feeling, known as a malocclusion, is a classic sign of TMD.
It doesn't mean your teeth have actually moved overnight. Instead, it’s a sign that the muscles controlling your jaw are in spasm, or that the joint itself is inflamed and swollen.
Think of your jaw muscles as a sophisticated pulley system designed to bring your teeth together perfectly. When those muscles get tight and exhausted from clenching, they can pull the jaw into a slightly new, strained position. That tiny shift is all it takes to make your bite feel completely foreign.
Key Insight: A sudden change in your bite is your body's way of telling you something is wrong. It's a signal that the jaw system is out of its natural alignment and being held in a stressed position by overworked muscles or an inflamed joint.
This feeling might be temporary—often at its worst in the morning after a night of clenching—or it can become a persistent problem. Either way, it’s a clear sign that your jaw is under a great deal of stress.
The image below shows how pain from a dysfunctional jaw joint can travel, causing symptoms that might not seem related at first.
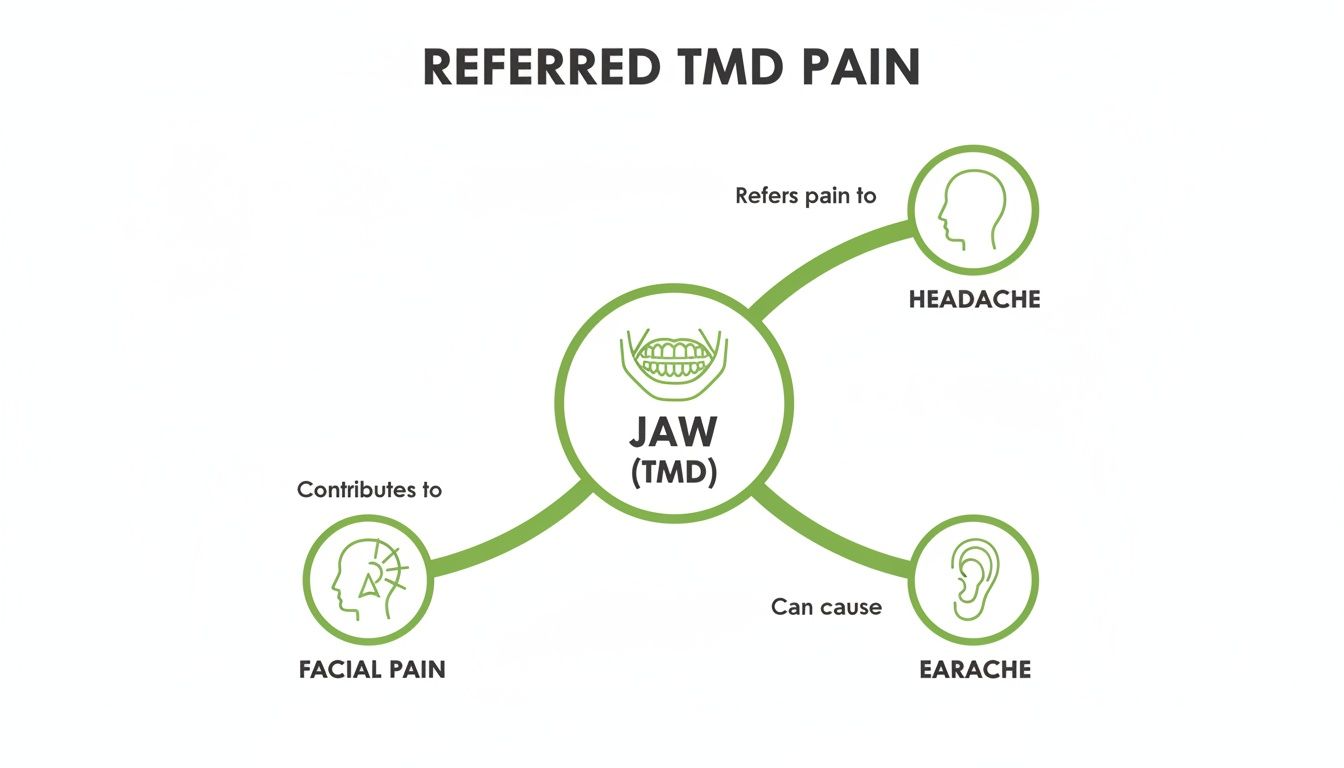
As you can see, the jaw is a central hub for nerves and muscles that can easily trigger headaches, earaches, and widespread facial pain.
The Destructive Cycle of Bruxism and TMD
While a misaligned bite is a problem during the day, what happens at night can be far more damaging. The link between TMD and sleep is powerful, often revolving around a condition called bruxism—the involuntary clenching or grinding of your teeth while you sleep.
Bruxism isn’t just a bad habit; it's a powerful engine that drives TMD pain. The massive forces created by nighttime grinding put extreme pressure on your jaw joints and exhaust the surrounding muscles. This leads to that all-too-familiar cascade of morning symptoms:
- Waking up with a stiff, achy jaw.
- Intense headaches, especially in the temples.
- New or worsening tooth sensitivity.
- Nagging facial, neck, and even shoulder pain.
Bruxism is a major factor in the TMD world. Research shows that nighttime teeth grinding is connected to TMD symptoms in 17% of cases worldwide, and that number jumps to an incredible 70% co-prevalence in North America. Sleep bruxism is a primary culprit for worsening facial pain in up to 30% of adults with TMD.
This creates a vicious cycle. The pain from TMD disrupts your sleep, and the poor sleep and grinding, in turn, make your TMD symptoms even worse. Breaking that cycle is the key to finding lasting relief.
The Deeper Link to Sleep Disordered Breathing
But the connection between TMD and sleep goes even deeper than bruxism. We’re now seeing an incredibly strong link between jaw dysfunction and sleep-disordered breathing, including conditions like obstructive sleep apnea (OSA).
Think of your airway as a soft, flexible tube. In some people, the lower jaw sits a little too far back, which can narrow this tube, especially when they lie down to sleep.
When the airway is partially blocked, the body's natural reflex is to thrust the jaw forward to open it up and let air in. This repetitive, unconscious jaw-jutting and clenching happens all night long as the body fights to breathe. While this instinct is protective, it puts a tremendous strain on the temporomandibular joints.
This constant nightly workout can directly cause or severely worsen TMD symptoms.
This is exactly why a comprehensive evaluation is so critical. Trying to treat jaw pain without checking the airway is like fixing a leaky pipe but ignoring the dangerously high water pressure. You might patch the immediate problem, but you haven't addressed the root cause. You can learn more about obstructive sleep apnea in our detailed guide.
Understanding the interplay between your bite, your sleep, and your breathing is a game-changer. It shows that effective treatment has to look beyond just the jaw to find a solution that truly lasts.
When Your Symptoms Warrant Expert Care
Knowing the signs of TMJ dysfunction is the first step, but recognizing when it's time to take action is what truly matters. While mild, occasional jaw discomfort might go away on its own, certain symptoms are clear signals that your body needs professional help.
These aren’t minor annoyances to be ignored; they are red flags pointing to a significant underlying issue.
Think of it like a "check engine" light in your car. You can ignore it for a little while, but doing so almost always leads to a much bigger problem down the road. Acting promptly is the key to preventing long-term complications and finally finding a path to lasting relief.
Critical Red Flags That Demand Attention
If you experience any of the following symptoms, it's time to stop waiting and seek a professional evaluation from a specialist. These signs indicate that the dysfunction is seriously affecting your daily life and joint health.
- A Locked Jaw: This is the most urgent red flag. Whether your jaw gets stuck open or you can't open it wide enough to eat, locking points to a severe mechanical failure within the joint.
- A Sudden Change in Your Bite: If your teeth suddenly feel like they don’t fit together correctly, it’s a big sign that muscle spasms or joint inflammation are pulling your jaw out of its natural alignment.
- Severe, Unrelenting Pain: Pain that disrupts your sleep, makes it difficult to eat, or interferes with your ability to work or focus is not normal and requires expert care.
- Pain Accompanied by Dizziness or Vertigo: Because the jaw joint is so close to the structures of the inner ear, severe inflammation can sometimes throw off your balance, causing dizziness or a spinning sensation.
- Grating or Grinding Sounds (Crepitus): While a painless click might be benign, a sandy or gravelly sound often means the cartilage in the joint is wearing down and bone is rubbing against bone.
These symptoms go far beyond general discomfort. They are definitive signs that your jaw system is in distress and needs a thorough diagnostic workup to get to the root cause.
Finding the Right Kind of Care
When facing these symptoms, many people start with their general dentist, which is a reasonable first step. However, the world of TMD is incredibly complex and often requires a much deeper level of expertise. While a dentist can identify basic issues, a TMD specialist brings a much broader perspective to the table.
A TMD specialist operates at the intersection of dentistry, neurology, and musculoskeletal health. Their focus isn't just on the teeth but on the entire system—joints, muscles, nerves, and even the airway—to understand why the symptoms are happening.
This specialized approach is crucial because the source of the problem is rarely just one thing. A specialist will conduct a detailed evaluation that goes far beyond a standard dental check-up.
What to Expect from a Specialist Evaluation
A comprehensive diagnostic visit with a specialist is designed to uncover the underlying drivers of your pain and dysfunction. This process demystifies your symptoms and builds a clear, actionable plan for your recovery.
The evaluation will likely include:
- Advanced Imaging: Specialized scans like a Cone Beam Computed Tomography (CBCT) scan provide a detailed, 3D view of your jaw joints, bones, and airway.
- Thorough Muscle Examination: The clinician will manually assess the muscles in your head, neck, and face to identify trigger points, tension, and patterns of referred pain.
- Joint and Airway Assessment: This involves evaluating your jaw’s range of motion, listening for joint sounds, and screening for signs of sleep-disordered breathing that could be contributing to the problem.
This detailed approach ensures that your treatment plan is not just a temporary fix. By identifying and addressing the root cause, you can find a path toward genuine healing and long-term well-being. To explore what these next steps might look like, you can learn more about modern TMJ treatment options that focus on root-cause solutions.
Your Top Questions About TMJ Symptoms Answered
Diving into the world of temporomandibular joint dysfunction can feel overwhelming, and it's completely normal to have a lot of questions. As you start connecting the dots between how you're feeling and a potential TMJ issue, you’re probably wondering what it all means.
We hear these questions all the time from our patients. Our goal here is to give you clear, straightforward answers that build on what you've learned and help you feel more confident about the road ahead. We’ll cover everything from whether this can clear up on its own to the role of surgery and how TMD shows up in younger patients.
Can TMJ Dysfunction Go Away On Its Own?
While a minor case of jaw soreness—say, after chewing something really tough—might fade with a little rest, chronic TMJ dysfunction rarely disappears without help. The underlying problems, like muscle imbalances, joint inflammation, a misaligned bite, or airway issues, don't just fix themselves. They tend to stick around and can even get worse.
Ignoring persistent symptoms of temporomandibular joint dysfunction like clicking, locking, or recurring headaches is a gamble. Think of it like a tire that's out of alignment on your car; the longer you drive on it, the more wear and tear you cause. A proactive approach, starting with a proper diagnosis and leading to targeted therapy, is the best way to find lasting relief and avoid long-term damage.
Is Surgery My Only Option for Severe TMJ Pain?
Absolutely not. In fact, surgery is a last resort, reserved for only a very small percentage of the most severe TMD cases. The vast majority of our patients find significant, lasting relief through conservative, non-invasive treatments that focus on healing the body's own structures.
Modern specialty clinics have moved past the old models of care. We prioritize regenerative and therapeutic options that get to the root cause of the dysfunction. The goal is to heal the joint, retrain the muscles that aren't working correctly, and restore proper jaw function—all without the major risks and downtime of surgery.
Modern Treatment Focus: Today’s most effective treatments center on non-surgical interventions that promote your body’s natural healing ability. This includes therapies like Prolotherapy, Platelet-Rich Fibrin (PRF) injections, cold laser therapy, and orofacial myofunctional therapy.
These approaches are all designed to help your body repair itself, offering a path to recovery that works with your biology, not against it.
How Do I Know if My Headaches Are Caused by TMD?
This is a huge one, since headaches are one of the most common—and disruptive—symptoms of TMD. The biggest clue is when your headaches show up with other classic TMD symptoms.
If your headaches often come with any of the following, there’s a good chance they’re connected:
- Jaw Tenderness: Is your jaw joint or the muscles in your cheeks sore to the touch?
- Facial Muscle Tightness: Do you feel a constant tension, especially in your temples?
- Joint Sounds: Are you hearing clicking or popping noises when you talk, chew, or yawn?
- Ear-Related Pain: Do you get aches in or around your ear that aren't from an infection?
Another tell-tale sign is a headache that just won’t quit, no matter what typical pain relievers you try. A comprehensive evaluation with a TMD specialist can finally confirm the connection and create a treatment plan that targets the real source of your pain.
Can Children and Teenagers Have TMJ Dysfunction?
Yes, TMD isn't just an adult problem. It absolutely affects children and adolescents, too. In younger patients, the causes are often tied to developmental issues, oral habits, or unresolved airway and breathing problems that have a domino effect on the jaw.
For example, habits like thumb sucking or nail biting can put a ton of stress on a developing jaw joint. A sports injury or accident can also be a trigger. Even more fundamentally, things like a restrictive tongue-tie can mess with oral posture and jaw development from a very young age, paving the way for future TMJ problems.
Getting an evaluation with a specialist early on is key. By stepping in at a younger age, we can help guide healthy jaw growth and function, preventing much more serious issues down the road.
At the Pain and Sleep Therapy Center, we specialize in finding the root causes behind your symptoms to deliver relief that lasts. If you're ready to stop chasing temporary fixes and find a real solution, schedule a consultation with our expert team today. Learn more at https://pscharlotte.com.