That clicking, popping, and constant ache in your jaw isn't just some random annoyance. It's your body sending a clear signal that the complex system connecting your jaw and skull is in distress. Finding real relief isn't about popping a painkiller; it’s about figuring out why it's happening. The key is to uncover the root cause—whether it’s chronic muscle tension, a misaligned joint, or even an airway issue—and use targeted, non-surgical therapies to get things back on track.
This approach goes way beyond temporary fixes. It’s about restoring proper function for good.
Understanding Your Jaw Pain and TMJ
If you're dealing with jaw pain, you're in good company, though it probably doesn't feel that way. The persistent discomfort, the frustrating clicks, and the headaches that sneak up on you can make simple things like chewing, talking, or even yawning feel like a chore. This experience is almost always tied to the temporomandibular joint (TMJ), one of the most sophisticated and hard-working joints in your entire body.
Think of your TMJ as a high-tech sliding hinge, responsible for all the up-and-down and side-to-side movements your jaw makes. When everything is working smoothly, you don't even notice it. But when the muscles, ligaments, and the joint itself get out of sync, you end up with a temporomandibular disorder (TMD). This isn't just one problem; it's a whole family of issues that can affect your jaw joint and the muscles that control it.
The Scope of the Problem
The impact of TMD is much bigger than most people realize. In fact, it's one of the most common and underrecognized health issues out there. Get this: nearly a third of the world's population—about 29.5%—struggles with some form of TMD. That’s a staggering number.
The data also shows that women are disproportionately affected, facing a 1.75-fold higher risk than men, which may point to underlying hormonal or structural factors. You can explore the full study on global TMD prevalence here.
What this statistic really means is that what you're feeling is real, it's significant, and it absolutely deserves a clear path to resolution.
Your TMJ is not an isolated component; it's a critical part of a larger system that includes your airway, posture, and nervous system. Effective treatment recognizes these connections and addresses the root cause, not just the noise your jaw makes.
Before we dive deeper, it can be helpful to connect the dots between what you're feeling and what it might mean. This quick guide can help you make sense of your symptoms.
Decoding Your TMJ Symptoms: A Quick Reference Guide
| Symptom | What It Feels Like | What It Could Mean | When to See a Specialist |
|---|---|---|---|
| Clicking or Popping | A distinct "click" or "pop" when opening or closing your mouth. Usually painless but can be loud. | The small cartilage disc inside the joint is slipping out of place and then popping back in. Common, but can worsen. | If the clicking is new, becomes painful, or is accompanied by jaw locking. |
| Jaw Locking | Your jaw gets "stuck" in an open or closed position, making it hard to move. | The disc has slipped completely and is blocking the joint's movement. This is a clear sign of dysfunction. | Immediately. Jaw locking can lead to more significant joint damage if left unaddressed. |
| Headaches & Migraines | Dull, aching pain in the temples, forehead, or back of the head, often worse in the morning. | The jaw muscles are overworked from clenching or grinding, radiating tension into the head and neck. | If you have frequent headaches that don’t respond to typical pain relievers, especially with other jaw symptoms. |
| Ear Pain & Fullness | A feeling of stuffiness, ringing (tinnitus), or aching in or around the ear. | The TMJ is located right next to the ear canal, and inflammation in the joint can affect the ear. | When an ear specialist has ruled out an infection and the pain persists, particularly with jaw movement. |
| Muscle & Facial Pain | A tired, sore feeling in your face, especially the cheeks and jawline. Pain can also spread to the neck and shoulders. | Your facial muscles are in a constant state of tension, often from clenching, grinding, or poor posture. | If the pain is chronic, affects your daily life (like eating), and doesn't improve with at-home care. |
This table is just a starting point, but if any of these symptoms sound familiar, it’s a strong indicator that it's time to get a professional evaluation.
Why a Modern Approach Is Essential
For a long time, the go-to TMJ "solutions" were pretty generic—think standard-issue nightguards or pain medication. While these can sometimes take the edge off, they rarely fix the mechanical or muscular problem causing the pain in the first place. A modern, specialized approach, like the one we take here at Pain and Sleep Therapy Center, goes much deeper.
We see TMD not just as a "jaw problem," but as a clue that points to other related issues, such as:
- Muscle Imbalance: When facial and neck muscles are overworked or strained, they can pull the jaw right out of its proper alignment.
- Joint Dysfunction: That little cartilage disc inside your joint can slip, which is what causes those classic clicking or locking sensations.
- Airway and Breathing Issues: Problems like sleep apnea often lead to intense nighttime teeth grinding (bruxism) as your body unconsciously struggles to keep your airway open.
- Postural Habits: Think about how many hours you spend with your head pushed forward at a desk. That posture puts a massive strain on your neck and jaw muscles, directly contributing to pain.
By understanding that your jaw pain is part of a complex dance between bones, muscles, and even your breathing, we can build a treatment plan that's more than just a temporary patch. Our goal is to demystify your symptoms, validate your experience, and give you a clear, reassuring path toward genuine, lasting healing.
Connecting Symptoms to Their Triggers
Knowing you have jaw pain is one thing, but making real progress starts when you connect the dots between your symptoms and their root causes. TMJ disorders rarely just show up one day. They’re usually the result of small, consistent strains that build up over time—kind of like a slow leak in a tire. You might not notice it at first, but eventually, the tire goes flat.
In the same way, persistent habits or even physical imbalances can slowly wear down your jaw's ability to cope until the pain finally breaks through. By taking a closer look at the type of pain or dysfunction you’re feeling, we can start to uncover the triggers keeping you in that cycle of discomfort. This is the key to creating a TMJ treatment plan that actually works.
Decoding the Signals Your Jaw Is Sending
Your jaw is trying to tell you something, and it usually communicates in three main ways: pain, mechanical issues, and sounds. Each one gives us a different piece of the puzzle.
-
Pain Signals: These are the most obvious cries for help. Chronic headaches, especially those wrapping around your temples like a tight band, are a classic sign. You might also have sharp earaches with no sign of an infection or a dull, aching pain that spreads through your face, neck, and even your shoulders. This is often your jaw muscles telling you they are exhausted and overworked.
-
Mechanical Issues: This is all about movement. A jaw that clicks or pops when you open your mouth is a sign that the small cushioning disc inside your joint is slipping out of place. If it gets worse and starts locking—where your jaw gets stuck open or closed—it means that disc is getting in the way of the joint moving smoothly.
-
Auditory Symptoms: Sometimes, the signals are sounds you hear. Tinnitus, that persistent ringing in your ears, can be linked to TMJ because your jaw joint sits right next to the delicate structures of your inner ear. When the jaw is inflamed and the muscles are tense, it can directly mess with your hearing.
This concept map shows just how interconnected the bones, muscles, and nerves of your jaw really are.
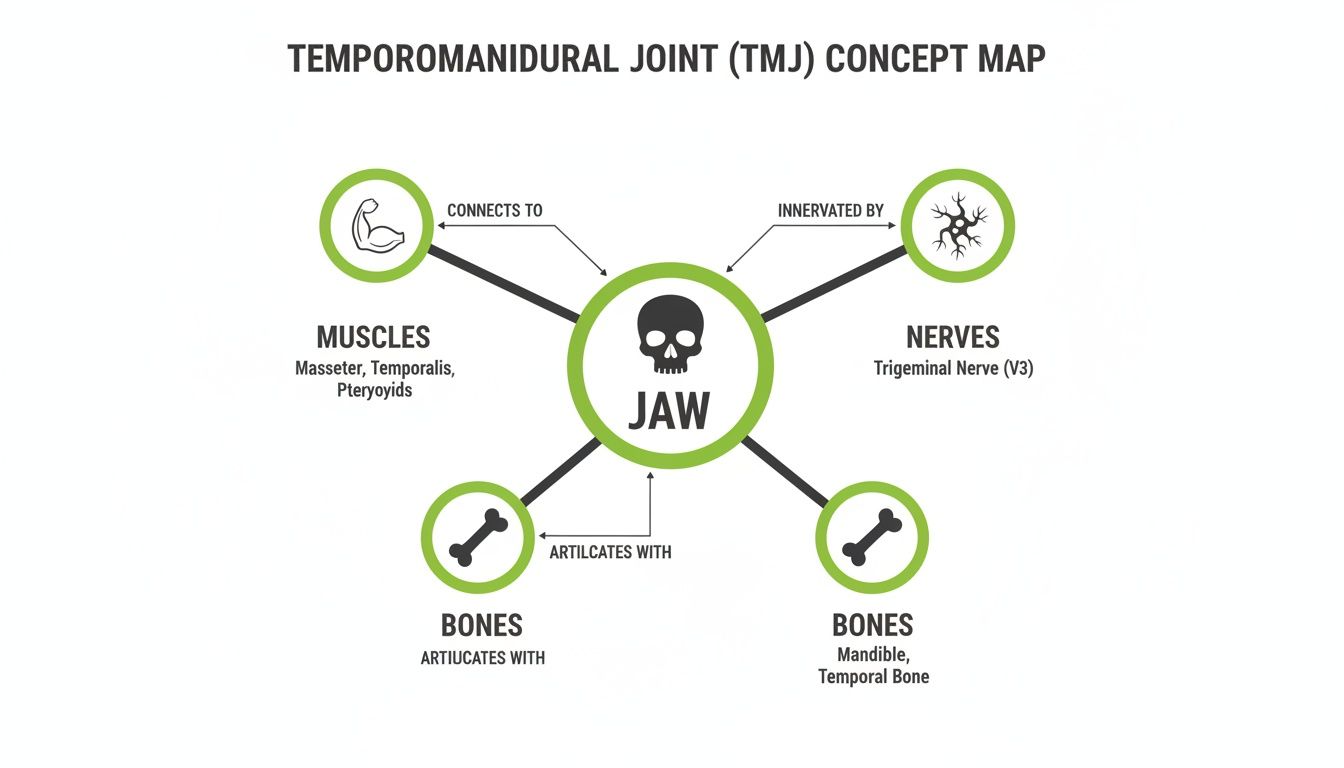
As you can see, a problem in one area—like overworked muscles—is going to have a ripple effect on the nearby nerves and the joint itself. It’s why TMJ symptoms can be so widespread and confusing.
Unmasking the Most Common Triggers
Once you've identified your main symptoms, the next step is to figure out what’s causing them. More often than not, the triggers are daily habits or underlying conditions that are putting way too much strain on your jaw.
Bruxism: Unconscious Clenching and Grinding
One of the biggest culprits behind TMJ pain is bruxism—the official term for clenching or grinding your teeth. So many of us do this without even realizing it, especially while we sleep. This habit can put hundreds of pounds of force on your teeth and jaw joints, which is why you might wake up with headaches, sore muscles, and even worn-down teeth.
A key insight here is that nighttime grinding often isn't just a "bad habit." It can be your body's way of trying to keep your airway open while you sleep, which points to a bigger issue like sleep-disordered breathing.
Stress and Its Physical Toll
When you’re stressed, your body tenses up. For many people, the jaw is the first place that tension goes. Think about how you might clench your jaw during a tough meeting or while sitting in traffic. When this becomes chronic, the constant muscle contraction leads to fatigue, inflammation, and pain that can radiate all over your head and neck.
The Impact of Poor Posture
Did you know your head weighs about 10-12 pounds? For every single inch your head drifts forward from a neutral position, it adds an extra 10 pounds of force on your neck and shoulder muscles. This "forward head posture" is incredibly common for anyone who works at a desk.
It forces your jaw muscles to work overtime just to hold your head up and keep your jaw in place. This constant strain is a direct path to TMJ problems, which is why addressing posture is a non-negotiable part of any lasting TMJ treatment plan.
Your Diagnostic Journey: What to Expect
Walking into a specialist’s office for jaw pain can be intimidating. The good news? The diagnostic journey for TMJ is less like a test and more like putting together a puzzle. We're not just looking at one piece; we're building a complete picture of your health to connect your symptoms to their real cause.
It all starts with a conversation. We’ll sit down and listen carefully as you describe what you're experiencing, whether it’s headaches, that frustrating jaw clicking, ear pain, or even fatigue. We'll also ask about your daily life—your work habits, stress levels, and sleep quality—because these details are often the biggest clues.
A Gentle, Hands-On Evaluation
After our chat, we’ll move on to a hands-on evaluation. This isn't about causing pain; it's a gentle process to see how your jaw is actually working. We'll watch how your jaw moves as you open, close, and slide it from side to side.
Next, the clinician will gently feel (palpate) the muscles around your jaw, face, head, and neck. This simple step helps us pinpoint specific areas of tenderness, tension, and inflammation. We're looking for the subtle signs, like muscle imbalances or uneven movement, that tell us how your entire head and neck system is functioning—or struggling to function—as a team.
Looking Beyond the Obvious Symptoms
A thorough diagnosis has to go beyond the jaw joint itself. At our center, we know that issues like poor posture or compromised breathing are often huge contributors to TMJ pain. We’ll take a look at your head and neck posture, checking for things like a forward head position that puts constant strain on your jaw muscles.
We will also evaluate your airway. This is a critical step because a restricted airway can lead to sleep-disordered breathing, a major trigger for the kind of intense nighttime teeth grinding that overworks the TMJ. This holistic view is the key to an accurate diagnosis and a tmj symptoms treatment plan that actually works.
Your diagnostic journey is about finding the 'why' behind your pain. A specialist isn't just looking at a sore joint; they are examining the interconnected system of muscles, nerves, posture, and even breathing that influences your jaw's health.
The numbers really show how common—and misunderstood—this condition is. In the United States, an estimated 1 in 12 adults (that’s about 35 million people) suffer from TMJ disorders. And that figure is likely low, since the symptoms are so often mistaken for simple headaches or ear pain.
Globally, the numbers are even more striking. Some studies show the prevalence reaching as high as 47% in certain regions, which highlights the urgent need for specialized centers that can provide an accurate diagnosis. You can discover more insights from this global meta-analysis.
Ultimately, this detailed diagnostic process ensures your treatment isn't just a generic solution. It’s a personalized roadmap built from a deep understanding of your unique anatomy, habits, and health history—paving the way for targeted therapies that deliver lasting relief.
Modern Non-Surgical and Regenerative Treatments
For a long time, TMJ treatment was mostly about managing the symptoms. Nightguards and pain relievers can quiet the pain, but they don't fix the underlying problem. Modern approaches, however, are geared toward something much more powerful: genuine healing.
Instead of just putting a bandage on the issue, these advanced therapies work to correct the mechanical problems and help rebuild damaged tissue from the inside out. This is where the real work of long-term relief begins.

Orofacial Myofunctional Therapy: Retraining Your Muscles
Think of Orofacial Myofunctional Therapy (OMT) as physical therapy specifically for your face, mouth, and tongue. It’s a series of targeted exercises designed to correct the poor muscle habits that contribute to TMJ pain. Many of us have developed dysfunctional patterns without even realizing it—things like incorrect swallowing, mouth breathing, or letting our tongue rest in the wrong spot.
An OMT specialist acts like a personal trainer for your face, teaching you how to retrain these muscles and correct your form. The exercises focus on key areas:
- Proper Tongue Posture: Training your tongue to rest gently against the roof of your mouth.
- Nasal Breathing: Shifting away from mouth breathing to reduce strain on the jaw.
- Correct Swallowing Patterns: Ensuring your tongue and facial muscles work together efficiently.
By establishing these correct habits, OMT helps stabilize the jaw joint, reduce muscle strain, and create better facial harmony. It's a foundational treatment that gives you the tools to maintain your jaw health for life.
Regenerative Medicine: Calling in Your Body’s Repair Crew
What happens when the jaw joint itself has sustained damage, like a stretched-out ligament or worn-down cartilage? This is where regenerative medicine comes in, offering a way to kickstart your body's natural healing process.
Imagine your joint is a construction site where the workers have all gone home. Regenerative treatments are like calling in a specialized repair crew—your body’s own healing cells—to get the job done right.
Two of the leading regenerative treatments for TMJ are:
- Prolotherapy: This involves injecting a natural solution (like dextrose) into the weakened ligaments around the TMJ. This creates a mild, controlled inflammation that signals your body to send growth factors to the area, strengthening and tightening the ligaments over time.
- Platelet-Rich Fibrin (PRF): PRF is a more advanced technique. We take a small sample of your own blood and spin it in a centrifuge to concentrate the platelets, white blood cells, and fibrin. This golden, gel-like substance is then injected directly into the joint, delivering a powerful cocktail of growth factors that speeds up tissue repair and reduces inflammation.
These options are a cornerstone of modern TMJ care because they promote true healing instead of just masking the pain.
The need for effective TMJ solutions has never been clearer. Myofascial pain, a key TMJ symptom, affects up to 85% of the global population at some point. This has fueled the growth of targeted treatments, particularly in the Americas, which held nearly half the market share. At Pain and Sleep Therapy Center, Dr. Greg Larson's team uses non-surgical regenerative therapies like Prolotherapy and PRF injections to address the root causes of TMJ pain and related conditions.
Cold Laser Therapy: A Gentle Push for Faster Healing
Cold Laser Therapy, also known as Low-Level Laser Therapy (LLLT), is a non-invasive treatment that uses specific wavelengths of light to penetrate deep into the tissues of your jaw joint. Unlike surgical lasers, this light doesn’t cut or burn. Instead, it gently stimulates your cells’ mitochondria—their tiny energy factories.
This cellular boost provides several key benefits:
- Reduces Inflammation: It helps calm the inflammatory process that causes so much pain and stiffness.
- Increases Blood Flow: Better circulation brings more oxygen and nutrients to the injured area.
- Accelerates Healing: By energizing the cells, it speeds up the body’s natural repair process.
Cold Laser Therapy is painless, quick, and combines beautifully with other treatments like OMT or regenerative injections to enhance their effects. It’s an excellent way to calm down a painful flare-up while supporting your body's long-term healing journey.
Comparing Modern Non-Surgical TMJ Treatments
To help you understand how these therapies fit together, we’ve created a simple comparison chart. Each treatment has a unique role, and they often work best when combined as part of a comprehensive, personalized plan.
| Treatment | Primary Goal | How It Works | Best For |
|---|---|---|---|
| Orofacial Myofunctional Therapy (OMT) | Correcting poor muscle habits and function. | A series of exercises to retrain tongue posture, breathing, and swallowing patterns. | Patients with dysfunctional habits like mouth breathing, tongue thrust, or incorrect swallowing that contribute to jaw strain. |
| Prolotherapy | Strengthening and tightening loose or injured ligaments around the jaw joint. | Injections of a natural irritant solution (dextrose) stimulate a healing response to repair connective tissue. | Individuals with joint instability, clicking, or popping caused by lax ligaments. |
| Platelet-Rich Fibrin (PRF) | Repairing damaged tissue (cartilage, ligaments, muscle) within the joint itself. | Injections of a concentration of the patient’s own blood platelets and growth factors to accelerate healing. | Patients with joint degeneration, arthritis, or significant inflammation and tissue damage. |
| Cold Laser Therapy (LLLT) | Reducing pain and inflammation while accelerating cellular repair. | Low-level light energy penetrates tissue to stimulate cellular metabolism and blood flow. | Anyone experiencing acute pain or inflammation; it enhances the results of other therapies. |
These modern, non-surgical approaches represent a significant step forward, offering a path to lasting relief by working with your body, not just on it.
At-Home Strategies for Immediate Relief
While getting to the root cause of TMJ dysfunction is the only way to find long-term healing, that doesn't mean you're powerless when a painful flare-up hits.
Having a solid toolkit of at-home strategies can bring immediate relief, ease muscle tension, and help you manage your symptoms day-to-day. Think of these techniques as first aid for your jaw—they won’t fix the underlying problem, but they can calm down an overworked system and give your joints a much-needed break.

The goal here is simple: soothe inflammation, release muscular knots, and stop doing things that make the pain worse.
Soothing Your Jaw with Temperature Therapy
One of the easiest and most effective ways to manage jaw pain is with temperature therapy. The trick is knowing when to use heat and when to use cold.
-
Moist Heat: For tight, sore, and achy muscles, applying a warm, damp cloth or a moist heating pad to the side of your face for 15-20 minutes works wonders. The moisture helps the heat penetrate deeper, which boosts blood flow and relieves that stubborn stiffness.
-
Cold Packs: If your pain feels sharp and you notice swelling, a cold pack is the way to go. Wrap an ice pack in a thin towel and hold it against the painful area for 10-15 minutes. This helps constrict blood vessels, which numbs the pain and brings down inflammation.
You can even alternate between the two, just be sure to give your skin a rest in between.
Gentle Movements to Restore Mobility
When your jaw hurts, the natural impulse is to keep it completely still. But sometimes, gentle and controlled movement can be exactly what you need to release tension and improve your range of motion. The key is to move slowly and never push into pain.
We’ve put together a guide with specific, safe movements you can do at home. Check out our TMJ pain relief exercises to learn how to carefully stretch your jaw muscles and promote relaxation without causing more strain.
A key principle of self-care is awareness. Pay attention to how your jaw feels throughout the day. Are you clenching while concentrating? Is your jaw tight when you wake up? This awareness is the first step toward breaking unconscious habits that contribute to your pain.
Making Smart Dietary Choices
What you eat can have a direct and immediate impact on your jaw pain. During a flare-up, the best thing you can do is give your jaw a vacation from hard work.
- Stick to Soft Foods: Think smoothies, yogurt, soups, and scrambled eggs.
- Avoid Chewy or Hard Items: Steer clear of tough meats, crunchy raw veggies, hard candies, and especially chewing gum.
- Cut Food into Small Pieces: This one simple step dramatically reduces the work your jaw has to do.
- Don't Open Wide: Be mindful of foods like big burgers or whole apples that force you to open your mouth wide.
These are temporary changes, but they can make a huge difference in your comfort level while your jaw is healing.
Managing Stress and Releasing Tension
The link between stress and jaw clenching is undeniable. When you’re stressed, your body tenses up, and for so many of us, that tension goes straight to the jaw.
This is why incorporating relaxation techniques into your daily routine is such a powerful TMJ symptoms treatment. Simple mindfulness practices, deep breathing exercises (like the 4-7-8 method), or even just a few minutes of quiet meditation can help calm your nervous system. This sends a signal to your jaw muscles that it’s safe to relax, helping you break that vicious cycle of tension and pain.
The Hidden Link Between Jaw Pain and Breathing
Have you ever considered that how you breathe—especially at night—could be the real reason behind your jaw pain? The connection between your airway and TMJ health is one of the most important, yet frequently missed, pieces of the puzzle when it comes to finding lasting relief.
When you can't get enough air while you sleep, your body goes into survival mode. One of its first instincts is to thrust the lower jaw forward to open up the airway. This protective reflex often leads to intense, unconscious teeth grinding and clenching, also known as bruxism.
This isn't a minor habit. The force your jaw can generate overnight is incredible, putting a massive strain on the jaw joints and surrounding muscles for hours on end. The result? You wake up with a sore, tight jaw, mysterious headaches, and a deep-seated exhaustion that no amount of coffee can touch.
Your Airway Is the Stairway to Health
This nightly battle for breath is a huge contributor to many TMJ disorders. If your body is constantly fighting just to breathe, your jaw never gets the chance to rest and heal. That's why a truly effective treatment plan has to look beyond just the jaw joint itself.
So many people who struggle with TMJ pain are also dealing with undiagnosed sleep-disordered breathing. Conditions from simple snoring to full-blown obstructive sleep apnea can trigger this protective grinding response. You can learn more about how specialists diagnose and treat these underlying sleep disorders to provide more complete care.
A restricted airway forces your body to prioritize survival over rest during sleep. The teeth grinding that follows isn't the actual problem—it's a symptom of your body's desperate attempt to keep you breathing. Getting to the root of the airway issue is fundamental to breaking the cycle of pain.
Retraining Your Breath for Jaw Relief
The good news is that you can take active steps to improve your breathing patterns, which in turn can bring direct relief to your jaw. There are simple but powerful techniques designed to retrain your body to prioritize efficient breathing through the nose.
One of the most well-known methods is the Buteyko Breathing Technique, which centers on gentle, controlled nasal breathing. Breathing properly through your nose encourages ideal oral posture—with your tongue resting on the roof of your mouth and your lips sealed. This small change helps stabilize the jaw, reduce muscle strain, and makes you far less likely to resort to mouth breathing at night.
By addressing the foundational link between your airway and your jaw, you can start tackling one of the biggest triggers of your TMJ pain. This integrated approach isn't just about managing symptoms; it’s about restoring the natural harmony between your breathing, sleep, and jaw health for relief that actually lasts.
Of course. Here is the rewritten section, crafted to sound like a human expert while following all the provided guidelines.
Your TMJ Treatment Questions, Answered
When you're dealing with jaw pain, it's completely normal to have a lot of questions. Getting clear, straightforward answers is the first step toward feeling confident about your treatment and finally getting relief. Let's walk through some of the most common questions we hear from patients.
How Long Will It Take for My Jaw to Feel Better?
This is probably the most common question we get, and the honest answer is: it depends. Every person’s situation is unique, so there’s no single timeline. However, many people feel a significant drop in pain within just a few weeks of starting therapies like Orofacial Myofunctional Therapy or cold laser therapy. These treatments are designed to calm down immediate inflammation and retrain muscle function.
On the other hand, regenerative options like Prolotherapy and PRF play the long game. They work by tapping into your body's own healing powers to rebuild and strengthen the joint. You can expect to see gradual but steady improvement over a few months. We’ll map out a personalized plan for you so you know exactly what to expect.
Should I Be Worried About My Jaw Clicking?
Not always. An occasional, painless click might just be a minor quirk in how your joint moves. But if that click comes with pain, locking, or you feel like your jaw is getting stuck, that’s a red flag. It’s a strong signal that you’re dealing with a TMJ disorder that needs a professional look.
When you have pain with the click, it often means the joint’s internal parts—like the small articular disc that acts as a cushion—are out of place. It can also mean the surrounding muscles are seriously overworked. Ignoring it can allow the problem to get worse, potentially leading to more damage down the road.
A professional diagnosis is the only way to be certain what’s causing the noise and discomfort.
Will Insurance Cover My TMJ Treatment?
Navigating insurance for TMJ treatment can feel tricky. Coverage varies wildly between medical and dental plans—some procedures might fall under one, some under the other, and some might not be covered at all.
Our administrative team is your best resource here. They’re pros at handling the paperwork and diagnostic codes needed to help you file claims and understand your benefits. We also offer flexible payment plans to make sure that financial worries don't stand in the way of you getting the care you need.
Can Kids and Teenagers Get TMJ Disorders?
Yes, absolutely. We see TMJ issues in children and adolescents quite often. In younger patients, the problem is frequently tied to other things, like underlying airway issues, habits such as thumb sucking, or a structural condition like a tongue-tie. Getting an evaluation early is key.
By addressing these root causes during their developmental years, we can often prevent more serious TMJ problems, sleep-disordered breathing, and the need for complex orthodontic work later on. If your child complains of jaw pain, grinds their teeth at night, or is a chronic mouth breather, it's a good idea to schedule a specialist evaluation.
At the Pain and Sleep Therapy Center, we believe in providing clear answers and effective, non-surgical solutions for TMJ pain. If you're ready to stop chasing symptoms and get to the root cause of your discomfort, schedule your consultation today. Learn more at https://pscharlotte.com.