When you hear "sleep apnea," the first thing that probably comes to mind is a CPAP machine. While it’s often treated as the default solution, it’s far from the only one. For many people, sleep apnea treatment without CPAP isn't just an alternative—it's a much better fit for their lifestyle. From simple oral appliances to targeted lifestyle changes, effective relief is possible for anyone who finds CPAP too difficult to use night after night.
Why CPAP Isn't the Only Answer for Sleep Apnea

CPAP therapy is incredibly effective, but there’s a catch: its success depends entirely on whether you can actually use it. The reality is that compliance rates can be surprisingly low. Studies show a significant number of people just give up on their machines. This guide is a practical roadmap to help you understand the full range of solutions out there.
We see patients seek alternatives for a few common reasons:
- Comfort and Claustrophobia: Let's be honest, wearing a mask all night can feel restrictive, uncomfortable, or even trigger anxiety.
- Noise and Disruption: The hum of the machine can be a real problem, disturbing not just you but your sleep partner as well. You end up trading one sleep issue for another.
- Travel and Portability: CPAP machines are bulky. For anyone who travels frequently, lugging one around is a major inconvenience that often leads to skipping treatment on the road.
- Maintenance and Upkeep: The constant cleaning and replacing of parts can feel like a chore that many people simply don't have time for.
The Critical Role of Adherence
Here’s the bottom line: the best treatment is the one you’ll actually stick with every single night. A CPAP machine collecting dust in a closet offers zero therapeutic benefit. This is precisely why exploring other options is so vital for your long-term health.
The goal of any treatment plan is consistent, restorative sleep. For many, the key to achieving this lies in finding a comfortable, sustainable alternative that fits seamlessly into their life, rather than forcing a one-size-fits-all solution.
This shift in thinking—from a single "gold standard" to a personalized approach—empowers you to have a much more productive conversation with a specialist. Understanding what is obstructive sleep apnea is the first step. From there, you can explore a treatment plan designed for your specific anatomy, lifestyle, and personal preferences.
Comparing Your Non-CPAP Treatment Options
If you’re looking for a sleep apnea treatment without CPAP, it’s easy to feel overwhelmed by the choices. But finding the right solution starts with understanding how each one works. Every approach tackles the problem from a different angle, varying in method, who it’s best for, and the level of commitment it requires.
The most effective and clinically recognized alternatives fall into a few key groups. These range from non-invasive, custom-fitted devices you wear at night to advanced procedures designed to address the specific anatomical reasons your airway closes.
An Overview of Leading Alternatives
Let's start with a high-level look at your options. Some treatments work by physically propping the airway open, while others focus on strengthening the muscles that support it or correcting the underlying structural issues causing the problem in the first place.
Here’s a quick introduction to the most common non-CPAP treatments we see:
- Oral Appliance Therapy (OAT): These are custom-made dental devices that gently reposition your jaw or tongue to keep the airway from collapsing. They are a frontline alternative for mild to moderate obstructive sleep apnea (OSA).
- Lifestyle & Positional Therapies: These methods address factors that contribute to sleep apnea. They include targeted weight management, simple aids to keep you from sleeping on your back, and specialized exercises to tone airway muscles.
- Hypoglossal Nerve Stimulation: Think of this as a pacemaker for your tongue. It’s an implantable device that delivers mild stimulation to keep the airway open while you sleep, typically reserved for moderate to severe OSA.
- Surgical Interventions: These are procedures that permanently change the anatomy of your throat, jaw, or nasal passages to create a wider, more stable airway for good.
The best treatment isn’t always the most aggressive one. Real success comes from consistent use and a measurable improvement in your sleep quality, which is why less invasive, more comfortable options are often the most effective in the real world.
To help you see how these options stack up, the table below gives you a clear, at-a-glance comparison. It breaks down each sleep apnea treatment without CPAP by how it works, what type of apnea it’s best for, and how invasive it is.
At-a-Glance Comparison of CPAP Alternatives
This quick summary compares the primary non-CPAP treatments, how they work, and their ideal use cases.
| Treatment Approach | Primary Mechanism of Action | Best Suited For (Apnea Severity) | Invasiveness Level |
|---|---|---|---|
| Oral Appliance Therapy | Mechanically repositions the lower jaw or tongue to open the airway. | Mild to Moderate | Non-Invasive |
| Positional Therapy | Uses devices to prevent sleeping on the back, where apneas are often worse. | Mild to Moderate (Positional OSA) | Non-Invasive |
| Weight Management | Reduces fatty tissue around the neck and throat, decreasing airway compression. | All Severities (especially with high BMI) | Non-Invasive |
| Myofunctional Therapy | Strengthens tongue and throat muscles through targeted exercises to improve airway tone. | Mild to Moderate | Non-Invasive |
| Hypoglossal Nerve Stimulation | An implanted device stimulates the nerve controlling the tongue to prevent collapse. | Moderate to Severe | Minimally Invasive |
| Skeletal & Nasal Surgery | Permanently alters bone or soft tissue structures to widen the airway. | Moderate to Severe | Invasive |
This framework gives you a solid foundation for making an informed choice. As we dive deeper into each of these options, you can refer back to this chart to see how all the pieces fit together in the bigger picture of getting healthy sleep without a CPAP.
A Deeper Look Into Oral Appliance Therapy

When people start looking for an effective sleep apnea treatment without CPAP, they often land on Oral Appliance Therapy (OAT). It’s a top contender for a reason. Instead of a machine and a mask, OAT uses a small, custom-fitted device that works with your body's own anatomy to keep your airway open all night long. It’s a powerful, patient-friendly solution that puts comfort and consistency first.
The most common device used in OAT is the Mandibular Advancement Device (MAD). You can think of it as a highly sophisticated mouthguard, but one that’s been precisely designed to get to the root cause of your obstructive sleep apnea. It’s only worn during sleep, making it a practical and unobtrusive path to breathing easier.
A MAD works on a simple but brilliant mechanical principle. It gently shifts your lower jaw slightly forward and down, creating just enough space behind your tongue and soft palate. This subtle adjustment prevents those tissues from collapsing and blocking your airway—the very thing that causes apnea events in the first place.
How Oral Appliance Therapy Works
Getting a custom MAD isn’t like buying a boil-and-bite guard at the pharmacy. It’s a precise medical intervention tailored to your unique anatomy, involving a close collaboration between you and a sleep medicine specialist.
The process is meticulous and involves a few key steps:
- Comprehensive Consultation: First, a specialist will thoroughly evaluate your airway, jaw structure, and teeth to see if you're a good candidate for OAT.
- Precise Digital Impressions: We use advanced scanning technology to create an exact 3D model of your mouth. This means no messy physical molds and a perfectly comfortable fit.
- Custom Fabrication: Your scans go to a specialized lab where your personal oral appliance is crafted from high-quality, medical-grade materials.
- Fitting and Calibration: Once your device arrives, you’ll come in for a fitting. Your specialist will make micro-adjustments to find that sweet spot between maximum effectiveness and total comfort.
This careful process ensures the device works as intended and is comfortable enough to wear all night, every night. Because the jaw’s position is so critical here, we always make sure everything is in proper alignment. This can sometimes overlap with understanding TMJ treatment options, as the two are closely related.
Ideal Candidates and Real-World Effectiveness
OAT is most often recommended for people with mild to moderate obstructive sleep apnea. It’s also an excellent alternative for those with severe OSA who just can't get used to CPAP therapy. An ideal candidate usually has healthy teeth and gums and is looking for a portable, hassle-free solution.
The clinical data behind MADs is compelling. A landmark 10-year study found that a remarkable 86% of patients using these devices maintained successful long-term results. While a CPAP machine might lower the Apnea-Hypopnea Index (AHI) more on paper, research shows both treatments deliver similar improvements in what really matters: quality of life metrics like reducing daytime sleepiness.
The true measure of a sleep apnea treatment’s success isn’t just its technical efficacy but its adherence rate. Because oral appliances are comfortable and easy to use, patient preference and nightly compliance are significantly higher compared to CPAP.
This real-world usage is what makes OAT such a powerful alternative. By providing a solution that patients can actually stick with, it delivers consistent, night-after-night relief. That means more restorative sleep and, ultimately, better overall health. For the right person, it’s a premier sleep apnea treatment without CPAP.
Exploring Lifestyle and Therapy-Based Solutions

While devices and appliances give you great mechanical support, some of the most effective forms of sleep apnea treatment without CPAP actually get to the root of why your airway collapses in the first place. These lifestyle and therapy-based solutions focus on changing the conditions that lead to apnea events, giving you sustainable, long-term relief by working with your body.
These aren't just about managing symptoms; they're about fundamentally improving your airway health. From simple changes in sleep posture to targeted muscle training, these methods let you take an active role in your own treatment. For many people, they can significantly reduce—or even resolve—sleep apnea.
The Power of Positional Therapy
For a lot of folks, sleep apnea gets dramatically worse when they sleep on their back. We call this positional obstructive sleep apnea, a condition where gravity simply lets the tongue and soft palate fall backward and block the airway. The fix can be surprisingly simple: Positional Therapy.
This approach uses basic tools—like special pillows or small wearable devices that vibrate gently when you roll onto your back—to train you to sleep on your side all night. It’s a completely non-invasive and easy-to-use strategy that directly counters the physical problem caused by back-sleeping.
While it's one of the most affordable non-CPAP options, its real strength lies in consistency. Comparative studies show that while a CPAP might lower apnea events more on paper, patients stick with positional therapy much better—using it for 2.5 hours longer each night. That real-world use is what matters, leading to an average drop of 7.4 sleep apnea events per hour and real improvements in daytime sleepiness. The Cleveland Clinic offers more insights on non-CPAP therapies like this one.
Weight Management and Airway Health
The connection between excess body weight and obstructive sleep apnea is undeniable. Fat deposits around the neck and throat can physically narrow your upper airway, making it much more likely to collapse when you sleep. Because of this, weight management is a foundational piece of any solid treatment plan.
Even a small amount of weight loss can make a huge difference. Losing just 10% of your body weight can lead to a major decrease in sleep apnea severity for many people. This strategy tackles the underlying anatomical pressure, making it a powerful and lasting solution.
For many patients, weight management isn't just a helpful add-on; it can be a primary treatment that reduces the need for other devices or therapies. It also makes any other treatment you pursue, from oral appliances to positional aids, even more effective.
Orofacial Myofunctional Therapy: An Exercise Program for Your Airway
Just like any other muscle, the muscles in your tongue, throat, and face can be strengthened through exercise. That’s the entire idea behind Orofacial Myofunctional Therapy (OMT), a kind of physical therapy designed specifically to improve how your airway works.
OMT involves a series of targeted exercises that retrain the muscles involved in breathing, swallowing, and even speaking. The goal is to correct poor habits (like mouth breathing), promote proper tongue posture (resting on the roof of your mouth), and ensure you're breathing through your nose. By improving the tone and coordination of these muscles, OMT helps them keep the airway open while you sleep.
This therapy is a proactive sleep apnea treatment without CPAP that addresses the function of your airway. It’s not a quick fix, but a structured program that builds lasting change from the inside out. You can learn more about how myofunctional therapy for sleep apnea works to retrain your muscles for healthier breathing.
These lifestyle and therapy-based solutions are often combined, creating a multi-pronged approach that delivers powerful results without a machine. By focusing on your posture, weight, and muscle function, you can build a stronger, more resilient airway.
Understanding Advanced and Surgical Pathways
When lifestyle changes, oral appliances, and therapy-based approaches don't bring enough relief, it's time to explore more advanced options. For people with specific anatomical issues or moderate to severe sleep apnea, these next-level treatments can offer powerful, and often permanent, solutions.
This represents a significant step up, targeting the root physical causes of airway obstruction with real precision. We're mainly looking at two categories here: neurostimulation and surgical correction. These aren't first-line treatments, but they are crucial for those who have tried other methods and need a more definitive resolution.
Hypoglossal Nerve Stimulation: A Pacemaker For Your Tongue
One of the most exciting developments in sleep apnea treatment is Hypoglossal Nerve Stimulation, probably best known by the brand name Inspire. Think of it as a pacemaker for your tongue.
This small, implantable device keeps an eye on your breathing patterns while you sleep. When it senses you're inhaling, it delivers a mild electrical pulse to the hypoglossal nerve, which controls your tongue's movement. This gentle stimulation nudges the tongue forward just enough to keep it from collapsing into your airway. It’s a smart system that syncs perfectly with your natural sleep cycle. You turn it on with a small remote before bed and off again in the morning.
So, who is this for? Ideal candidates typically have moderate to severe obstructive sleep apnea, have already tried and struggled with CPAP, and fall within a specific body mass index (BMI) range. A specialist will perform a drug-induced sleep endoscopy (DISE) to see exactly how your airway collapses, confirming if this technology is the right fit for you.
Surgical Interventions: Correcting Anatomical Obstructions
For some people, the cause of their sleep apnea is a clear, correctable anatomical issue. In these cases, surgery can provide a permanent fix by physically altering the structures that are blocking the airway. These are highly specialized procedures tailored to your specific anatomy.
Common surgical approaches include:
- Uvulopalatopharyngoplasty (UPPP): This procedure removes excess tissue from the soft palate and uvula, widening the airway at the back of the throat.
- Maxillomandibular Advancement (MMA): A more involved surgery, MMA moves the upper and lower jaws forward to create significantly more space in the entire airway.
- Nasal Surgery: Procedures like septoplasty can fix a deviated septum, improving airflow through your nose and reducing the negative pressure that can cause the throat to collapse.
The decision to pursue surgery is a big one. It's often based on the idea that a one-time intervention could eliminate the need for nightly management with a device.
Choosing surgery requires a careful evaluation by an ENT or oral surgeon, but when the right patient is matched with the right procedure, the results can be remarkable. In fact, surgical intervention has shown some of the highest success rates among all non-CPAP options, with certain procedures achieving cure rates of up to 86%. You can learn more about the high success rates of surgical sleep apnea treatments to see how they stack up.
How to Choose the Right Path for Your Health
Navigating the world of non-CPAP sleep apnea treatments can feel overwhelming. The truth is, the "best" solution is always the one that fits your specific needs, anatomy, and lifestyle.
It’s not about finding a single magic bullet. It’s about discovering the right fit for you. The choice depends on things like the severity of your apnea, your unique airway anatomy, and what you’re willing to commit to long-term. Making a smart decision starts with a clear understanding of your priorities and a collaborative approach with a specialist who can pinpoint the real cause of your sleep issues.
Key Factors in Your Decision
When you're comparing your non-CPAP options, it helps to think through a few key questions. This clarity will make your conversations with a sleep specialist much more productive and guide you toward a treatment you can actually stick with.
Ask yourself these questions for each potential therapy:
- Severity Alignment: Is this treatment clinically proven for my level of sleep apnea—mild, moderate, or severe? An oral appliance, for instance, is a fantastic frontline choice for mild to moderate OSA, but something like nerve stimulation is typically reserved for more severe cases.
- Lifestyle Compatibility: How will this fit into my daily life? If you travel a lot for work, a portable oral appliance is far more practical than trying to keep up with nightly exercises or planning around recovery from surgery.
- Comfort and Adherence: Let's be realistic. Are you more likely to use a simple positional device every single night than commit to a daily muscle-training routine? Consistency is the most important factor for success, so honesty here is key.
- Invasiveness Level: Are you looking for a non-invasive solution like myofunctional therapy, or are you open to a minimally invasive procedure like Inspire for a more permanent fix? Your comfort level with medical procedures is a huge part of the decision.
The ultimate goal is to move from just gathering information to taking decisive action. A personalized treatment plan gives you a clear, actionable path toward a comfortable, sustainable solution for better sleep and renewed health.
The Patient-Focused Process at Our Center
Finding the right sleep apnea treatment without CPAP is a partnership between you and your healthcare team. Here at the Pain and Sleep Therapy Center, our process is designed to be thorough, collaborative, and focused entirely on you. We just don't believe in one-size-fits-all solutions.
Our approach always starts with a comprehensive consultation and advanced diagnostics. We go way beyond a simple diagnosis to understand the "why" behind your airway obstruction. This deep dive allows us to identify the specific anatomical and functional issues causing your sleep apnea. From there, we work directly with you to co-design a treatment plan that aligns with your health goals and lifestyle.
This decision tree gives you a visual for how pathways to advanced treatments, like nerve stimulation or surgery, are considered after other methods have been explored.
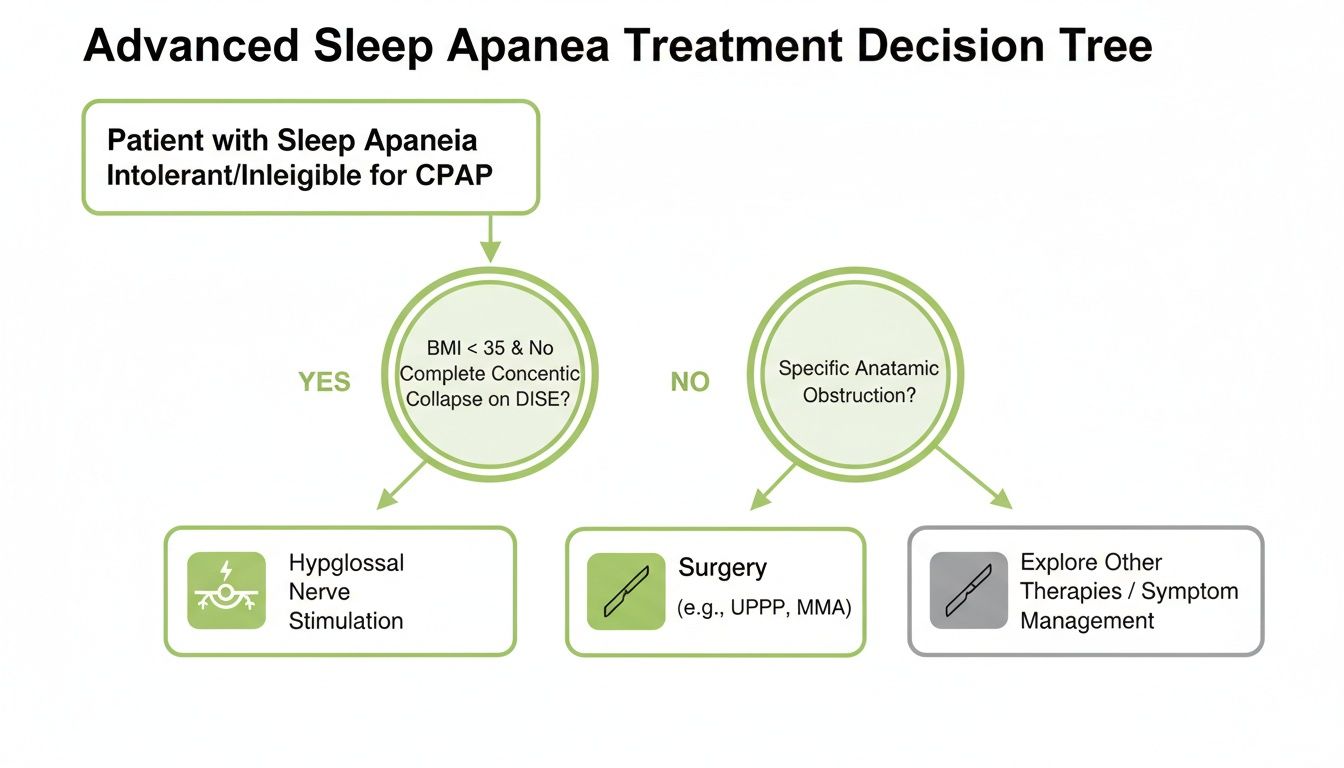
As the chart shows, the choice between these more advanced options comes down to a careful evaluation of a patient's specific condition and anatomy.
Whether that means a custom-fit oral appliance, targeted myofunctional therapy, or a referral to one of our trusted surgical partners, every recommendation is based on a complete picture of your health. Our mission is to empower you with the knowledge and tools you need to reclaim your sleep and improve your quality of life. The journey to better breathing and deeper rest starts with a clear, personalized strategy.
Questions We Hear All the Time About CPAP Alternatives
When you're exploring sleep apnea treatment beyond a CPAP machine, it’s natural to have questions. Getting clear, honest answers is the first step toward making a confident decision about your health and finally getting the restful sleep you need. We've put together some of the most common questions we hear from patients to help guide you.
Think of this as your starting point for a productive conversation with a sleep specialist. Our goal is to give you the knowledge you need to feel empowered in that discussion.
Can an Oral Appliance Really Work as Well as a CPAP?
This is probably the number one question people ask. For many with mild to moderate obstructive sleep apnea, the answer is a clear yes. These custom-fitted devices are often just as effective at managing symptoms like daytime fatigue and can dramatically improve your quality of life.
While a CPAP machine might produce a lower Apnea-Hypopnea Index (AHI) score in a sleep lab, that's not the whole story. Real-world success comes down to consistent use. Because oral appliances are so much more comfortable and convenient, patients actually use them—and that consistency often leads to better long-term health outcomes.
The best treatment is the one you’ll actually use every night. High compliance rates are why oral appliances often outperform a CPAP machine that’s been left to gather dust in a closet.
Will Insurance Cover Treatments Other Than CPAP?
This is another practical and important concern. The good news is that most medical insurance plans, including Medicare, do provide coverage for custom-made oral appliances. They are typically covered as a first-line treatment for mild to moderate OSA.
For severe OSA, they are also frequently covered if you’ve been diagnosed as CPAP-intolerant—meaning you’ve tried and failed to use a CPAP machine. Coverage for other options like positional therapy or surgery can vary, so it’s always smart to check with your insurance provider. We can help you navigate this process to make sure you understand your benefits.
How Do I Choose the Right Treatment for Me?
With several options on the table, patients often wonder how to make the right choice. The answer is simple: this decision should always be guided by a professional diagnosis from a sleep specialist. There is no one-size-fits-all solution, and what works beautifully for one person might not be a fit for another.
A sleep specialist will perform a comprehensive evaluation that includes:
- A deep dive into your sleep study data to understand the severity and specifics of your apnea.
- An examination of your unique airway anatomy to pinpoint the physical cause of the obstruction.
- A conversation about your lifestyle and preferences to find a solution you can stick with long-term.
This detailed assessment is the key to creating a personalized sleep apnea treatment without CPAP. It ensures your plan is built around your specific needs, giving you the best possible chance for success.
At Pain and Sleep Therapy Center, our team is dedicated to finding the root cause of your sleep issues and designing a personalized plan that works for you. Learn more about our patient-focused approach by visiting us at https://pscharlotte.com.