If you're worried about your child's feeding, speech, or sleep, you're not alone in wondering if tongue tie might be the culprit. It's a question I hear all the time from concerned parents.
So, how do you actually check for it? You can start by looking for some functional signs—like feeding difficulties or speech issues—and even do a gentle at-home assessment of how well the tongue moves. A classic sign is whether the tongue can lift freely to the roof of the mouth without forming a little heart shape at the tip.
But these are just clues. The most important thing to remember is to prioritize function over appearance before you jump to any conclusions or seek a professional diagnosis.
Is It Tongue Tie? What Parents Should Look For First
That little band of tissue under the tongue, the lingual frenulum, can cause big problems when it's too short or tight. This condition, known as ankyloglossia, can limit the tongue's range of motion and interfere with some of life’s most basic functions.
It’s so tempting to just peek inside your child’s mouth for a quick look, but honestly, that approach can be really misleading. A frenulum that looks tight might not cause any problems at all, while a much less obvious restriction could be the real source of significant challenges. The way we think about tongue tie has shifted dramatically away from just what we can see.

The Shift from Appearance to Function
Not too long ago, tongue tie was diagnosed almost entirely by how it looked. This visual-first method led to a lot of confusion and inconsistent diagnoses.
In fact, a 2020 meta-analysis of over 24,000 infants revealed something telling: the prevalence of tongue tie jumped from 7% with a simple visual exam to 10% when a standardized tool measuring function was used. This really drives home a critical point—how you check for tongue tie dramatically changes how often it’s correctly identified. You can dig into the full study on tongue tie prevalence and assessment if you're curious.
This guide is designed to help you spot the meaningful signs right at home. We're going to focus on observable red flags that point to actual limitations, moving beyond just a quick glance.
The most important thing to remember is that we prioritize function over a quick visual check. The goal isn't just to see a restriction but to understand how it impacts your child's ability to eat, speak, and breathe comfortably.
Quick Reference Red Flags for Tongue Tie
Before we get into the nitty-gritty of what to look for, it helps to have a quick overview of the common symptoms at different ages. This table sums up the key indicators that parents often notice first, helping you connect what you're seeing to potential underlying issues.
| Symptom Area | Infants (Feeding) | Toddlers & Children (Speech & Eating) | All Ages (Breathing & Sleep) |
|---|---|---|---|
| Common Signs | Poor latch, clicking sounds, milk dribbling, prolonged feedings, maternal nipple pain. | Picky eating (especially with textures), frequent gagging or choking, difficulty with sounds like 't', 'd', 'l', 's'. | Chronic mouth breathing (day and night), snoring, restless sleep, audible gasping or pauses in breathing. |
Starting with these observable, everyday signs helps you build a much clearer picture of what's going on with your child's oral function. This approach gives you a solid foundation for a more informed conversation with a healthcare professional, making sure you’re focused on solving the right problems from the start.
Next, we'll dive deeper into these functional signs.
Spotting Functional Signs During Daily Routines
Some of the most telling clues about a potential tongue-tie don't require you to look inside your child's mouth at all. They often hide in plain sight during your everyday routines. By observing how your child’s tongue functions during feeding, eating, and even sleeping, you can gather invaluable insight.
These functional signs are the real-world evidence that something might be getting in the way of their natural development.
Reading the Signs During Infant Feedings
For babies, feeding time is the main event where these signs surface. A healthy, efficient feeding should be a relatively calm and quiet experience for both you and your baby. When a tongue is restricted, however, it can really disrupt the process.
Pay close attention to what you hear during a feed. Is there a clicking or smacking sound? That’s a classic sign. It happens when the tongue can’t maintain a proper seal on the breast or bottle, causing the suction to constantly break and re-engage.
You might also see milk dribbling from the corners of their mouth, no matter how you adjust their position. This is another giveaway that the seal isn't strong enough. These seemingly small issues can cascade into bigger problems.
- Marathon Feedings: A baby with an inefficient suck might feed for 45 minutes or more but still act hungry right after. They're working hard but not transferring milk effectively.
- Constant Fussiness: If your baby is always pulling away, arching their back, or crying during feeds, it could be from pure frustration and exhaustion.
- Painful Gas and Reflux: When the seal breaks, a baby swallows a lot of air along with their milk—a condition known as aerophagia. This is a major cause of gas, spit-up, and reflux-like symptoms.
For nursing mothers, the signs are often physical and painful. A shallow latch from a tongue-tie can cause significant nipple pain, cracking, or even bleeding. You may also notice your nipples look compressed or misshapen—like the tip of a new lipstick—right after a feed.
Observing Toddlers and Older Children
As kids get older, the challenges of a tongue-tie simply change shape. Mealtimes and conversations become the new arenas where tongue mobility is put to the test.
With toddlers and older children, watch how they handle different types of food. A child with a restricted tongue often struggles to move food around their mouth to chew it properly. This can show up as:
- Picky Eating: They might start refusing chewy foods like meat or certain vegetables, sticking only to soft foods that are easier to manage and swallow.
- Messy Eating: Does an unusual amount of food seem to fall out of their mouth? This can happen when the tongue can’t effectively contain and guide food back for chewing.
- Gagging or Choking: Difficulty managing food can lead to frequent gagging or even scary choking episodes.
A key takeaway for parents of older children is that speech is just one piece of the puzzle. How a child eats, breathes, and sleeps paints a much more complete picture of their oral function.
Speech and Breathing Patterns to Watch For
The tongue's role in clear speech is massive. It has to move with speed and precision to form specific sounds. A tongue-tie can make this difficult, leading to trouble with sounds that need the tongue tip to lift to the roof of the mouth, like 't,' 'd,' 'l,' 's,' and 'r'.
Beyond eating and talking, one of the most significant and overlooked signs is your child’s resting posture. Take a look when they're relaxed and watching TV or sleeping. Is their mouth hanging open? Chronic mouth breathing is a huge red flag.
Ideally, the tongue should rest suctioned against the roof of the mouth, which naturally encourages nasal breathing. If a tongue-tie physically prevents this, the mouth has to drop open to maintain an airway. This can affect everything from sleep quality to facial development. Learning more about the importance of proper tongue posture can help you connect these dots.
Noticing these daily functional signs is the first, most important step in figuring out if your child needs a professional evaluation.
A Gentle Guide to Checking Tongue Mobility at Home
Once you've started noticing some of the functional red flags in daily life, you can do a gentle, at-home check of your child's tongue mobility. The key here is to be curious and careful, making it a calm and even playful experience.
Remember, this isn't about making a diagnosis. It's about gathering clues and observing how your child's tongue moves. The goal is simply to observe—never force a movement or cause any distress.
For an infant, the 'tongue sweep' is a simple and effective method. With a clean finger, gently trace along your baby's lower gum line, moving from one side to the other. A tongue with good mobility will often follow your finger, showing smooth side-to-side (lateral) movement. You’re just looking for a nice, coordinated motion.
If the tongue seems stuck in the middle or has trouble crossing the midline, that could be a clue. It’s also helpful to peek inside your baby’s mouth right after a feed or when they're relaxed and happy. Gently encourage them to open up and see if the tongue lifts freely when they cry or coo. Does it elevate easily, or does it seem to stay low and flat?
Turning Observation into a Game for Toddlers
With a toddler or older child, you can turn this whole process into a fun game. This approach takes away any pressure and makes them much more likely to cooperate. Kids are usually happy to play along.
Here are a few games you can try:
- Reach for the Sky: Ask your child to open their mouth wide like a lion and try to touch the roof of their mouth with the tip of their tongue. A restricted tongue might struggle to lift high, or you might see it dip in the middle as it strains.
- Catch the Crumb: Place a tiny bit of soft, safe food (like a single sprinkle or a dot of yogurt) just behind their top front teeth and ask them to lick it off. This little test shows if they can lift the tip of their tongue without having to move their whole jaw.
- Funny Faces: This one is a classic. Take turns making silly faces in a mirror and ask them to stick their tongue straight out as far as it can go. Pay close attention to the shape of the tip. A restricted tongue often forms a very distinct heart shape or has a little divot in the middle because the frenulum is pulling the center down.
These simple, playful interactions can give you a surprising amount of information about how freely their tongue can move.
Remember, a single observation isn't conclusive. It’s the combination of functional signs—like feeding issues or speech difficulties—and observations from these gentle checks that builds a compelling case for seeking a professional opinion.
Understanding the Bigger Picture
It’s helpful to know just how common these issues are. Global prevalence estimates for tongue-tie in newborns now range anywhere from 0.1% to 15%, but most studies land somewhere between 5% and 10%.
A major 2020 review found an 8% prevalence in infants under one year old, affecting nearly twice as many boys as girls. Here's a critical finding from that same study: when clinicians used standardized assessment tools, they identified tongue-tie in 10% of babies. But when they relied on a quick visual inspection alone, that number dropped to 7%. You can learn more about these tongue-tie findings and their implications.
This data really drives home the point that a functional assessment—like the gentle checks you're doing—is more in line with modern diagnostic standards than just a quick look.
The flowchart below shows how these restrictions can ripple out and affect key areas of a child's development.
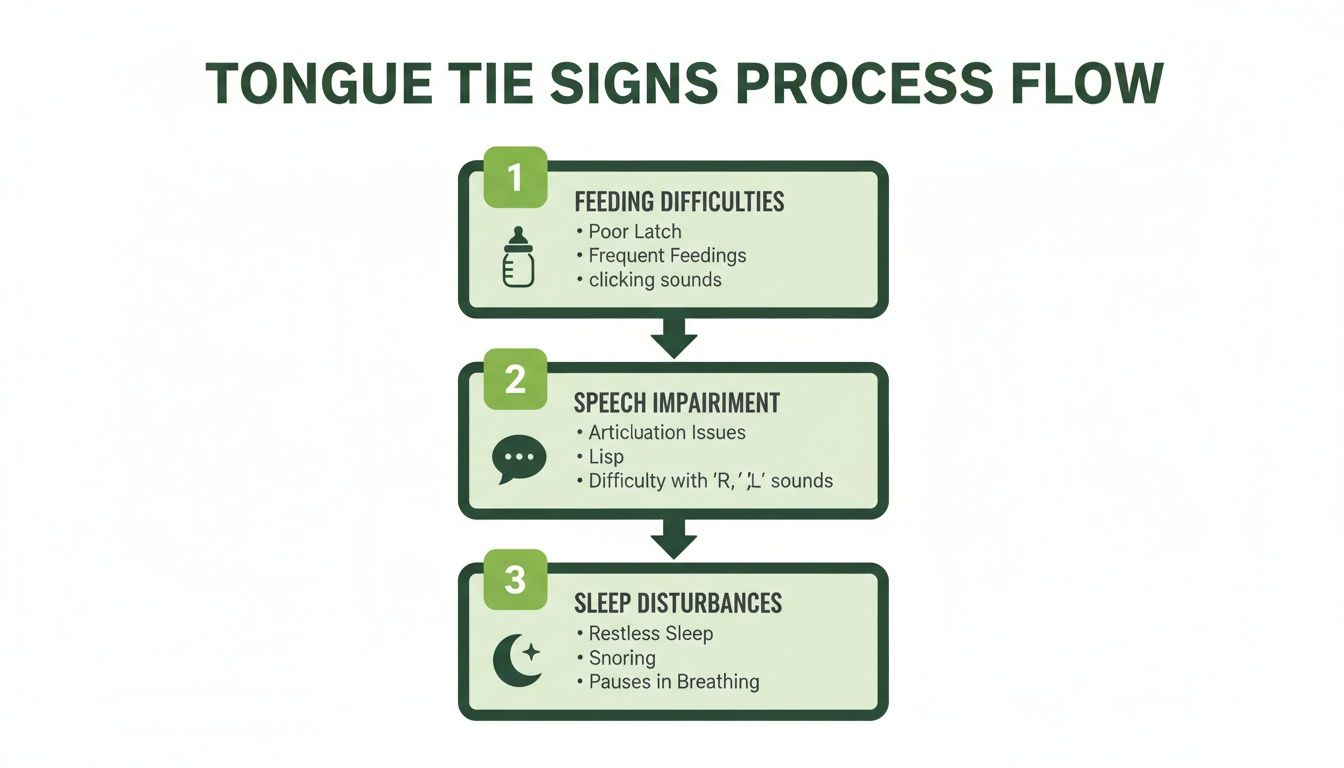
This process flow highlights that what might start as a feeding challenge can later show up as speech issues or even disrupt healthy sleep patterns, showing just how interconnected oral function is.
When Your Home Check Suggests a Professional Evaluation
Your at-home observations are an invaluable starting point, but they're really just pieces of a much larger puzzle. If your gentle checks and daily monitoring consistently point toward a functional limitation, that’s a clear signal to take the next step: a professional evaluation. Getting a formal diagnosis isn’t something you can do at home—it requires the expertise of a specialist trained in oral function.
Making that appointment can feel a little daunting, but certain scenarios make the need for a professional opinion much clearer. If you've been working hard with a lactation consultant but feeding issues just won't resolve, or if a speech therapist has pinpointed specific articulation problems tied to tongue mobility, it’s time.
The same goes for any signs of sleep-disordered breathing. Things like chronic snoring, really restless sleep, or audible gasps for air are significant red flags that absolutely warrant a specialist's assessment. These issues can have long-term impacts, and an evaluation can help get to the root cause. You can learn more about how myofunctional therapy addresses sleep apnea and related breathing issues in our detailed guide.
What to Expect from a Specialist Assessment
A professional evaluation is so much more than a quick peek inside your child's mouth. A trained provider—often a pediatric dentist, ENT, or a specially trained physician—will conduct a detailed assessment that looks at both the anatomy and the function. They’ll listen to all your concerns, review your child's history, and perform a careful, hands-on examination.
The whole process is designed to be objective and data-driven, moving way beyond a simple visual check. The goal is to understand precisely how any oral restrictions are impacting your child's ability to eat, speak, and breathe the way they should.
The Tools of the Trade for Accurate Diagnosis
To get an accurate diagnosis, specialists rely on standardized tools and classification systems. This approach removes the guesswork and provides measurable data, which is crucial for figuring out if a procedure is genuinely necessary.
Two of the most well-regarded instruments include:
- The Hazelbaker Assessment Tool for Lingual Frenulum Function (HATLFF): This is a comprehensive scoring system that evaluates both the appearance and the function of the tongue. It assigns points for things like tongue lift, extension, and side-to-side movement, giving a clear, quantifiable result.
- Kotlow's Classification and the Coryllos Classification System: These systems are used to grade the severity of a tongue-tie based on where the frenulum attaches to the tongue and the floor of the mouth. They give clinicians a consistent way to describe the anatomical restriction.
By using these established tools, specialists can confidently tell the difference between a frenulum that simply looks tight and one that is genuinely causing a functional problem.
A professional evaluation is about connecting the dots. It links the symptoms you see at home—like a poor latch or speech delays—to the physical limitations found during a structured, functional assessment. This ensures treatment is recommended only when truly needed.
Why a Thorough Evaluation Matters
The push for more rigorous, function-based screening has become incredibly important. Over the last couple of decades, shifts in how clinicians check for tongue-tie have led to a huge rise in diagnoses and surgical procedures. In the United States, data from 1996 to 2012 revealed a roughly seven-fold increase in diagnosed ankyloglossia and a ten-fold increase in frenotomies among infants.
This trend really highlights the need for a comprehensive evaluation that assesses feeding efficiency, nasal breathing, and compensatory muscle strain before jumping to a procedure. You can read more about these findings on the rise in tongue-tie diagnoses and the call for better screening.
This kind of careful, measured approach helps prevent unnecessary interventions and ensures that if treatment is recommended, it directly addresses the functional challenges your child is facing. It's the best way to create a clear and effective path forward.
Understanding the Path to Treatment and Recovery
Getting a tongue-tie diagnosis for your child can feel overwhelming, but the good news is that the path to treatment is well-established and focused on restoring function. What comes next isn't just a simple procedure; it's a collaborative effort to ensure your child’s long-term success. It’s all about creating the right conditions for their tongue to finally learn how to move correctly.
The main treatment for a significant tongue-tie is a frenectomy, a procedure that releases the tight band of tissue (the lingual frenulum). This simple release gives the tongue the freedom it's been missing, paving the way for the full range of motion needed for feeding, speaking, and even proper breathing.

The Modern Frenectomy Procedure
These days, many top providers use a specialized soft-tissue laser for frenectomies. This modern approach has some serious advantages over the old-school scissor or scalpel methods.
A laser frenectomy is incredibly precise and fast—it’s often over in less than a minute. As the laser works, it seals the blood vessels, which means there’s minimal to no bleeding. This also cuts down on post-procedure swelling and discomfort, making the healing process much smoother and quicker for your child.
For babies, a little topical numbing gel is usually all that’s required. In most cases, they can feed right after the procedure is done. This isn't just for comfort; it’s actually the very first step in helping them use their newly freed tongue.
Why the Procedure Is Only the Beginning
This is so important to understand: the frenectomy itself is just the first step. Think of it like taking a cast off a broken arm. The physical restriction is gone, but the muscles are weak and have no idea what to do. A tongue that’s been tied since birth has developed all sorts of compensatory habits and has never learned to function properly.
The release creates the opportunity for correct function, but it does not guarantee it. True, lasting success depends on a team-based approach that includes therapy and diligent aftercare to retrain the tongue's muscles and prevent the tissue from reattaching.
This is where the real work starts. A good treatment plan doesn’t just snip the tissue; it addresses the root cause of the functional issues. Without that critical follow-through, the benefits of the procedure can be short-lived.
Building Your Collaborative Care Team
A successful outcome almost always relies on a team of specialists working together. The procedure alone isn't enough; therapy is essential for teaching the tongue its new job.
Your team will likely include:
- The Releasing Provider: This is the dentist, ENT, or physician who actually performs the frenectomy.
- A Lactation Consultant (IBCLC) or Feeding Therapist: For infants, this person is your guide. They help your baby relearn how to latch and feed efficiently now that their tongue can move.
- An Orofacial Myofunctional Therapist (OMT): Think of an OMT as a physical therapist for the tongue. For older children (and sometimes babies), they provide specific exercises to build tongue strength, establish correct swallowing patterns, and ensure proper oral rest posture.
This team approach ensures every piece of the puzzle is addressed, from the initial release to the final stages of muscle retraining.
The Critical Role of Post-Procedure Care
After the frenectomy, your provider will give you a specific set of active wound management exercises. These aren't optional suggestions—they are just as important as the procedure itself.
The goal here is twofold. First, these gentle stretches prevent the wound from healing back together, a problem known as reattachment. Second, they encourage the tongue to explore its new range of motion, helping to build new neural pathways for correct movement. You’ll need to do these consistently for several weeks.
Alongside these stretches, therapy is key. For older children, learning orofacial myofunctional therapy exercises is how you reprogram their muscle memory. This therapy helps them unlearn old habits—like using their cheeks to swallow—and master new, efficient patterns for eating, speaking, and breathing. This is what truly resolves the underlying issues for good.
Your Top Tongue Tie Questions, Answered
When you first hear the term "tongue tie," it can open the door to a dozen more questions. It's completely normal to feel a bit overwhelmed. As a parent, you just want clear, straightforward answers to help you make the right choice for your child.
We hear the same concerns from families every day. Let's walk through the most common questions we get, so you can feel more confident about your next steps.
Will a Tongue Tie Fix Itself?
This is probably the number one question parents ask, and it comes from a place of hope. But the short answer is no—a functionally significant tongue tie won't resolve on its own.
The tissue under the tongue, the lingual frenulum, is made of tough collagen. It’s more like a little rope than a rubber band, so it doesn't just stretch out over time. When left alone, a baby will learn to work around the restriction. They might start using their jaw or cheek muscles to eat instead of their tongue, which can lead to other issues down the road like jaw pain, dental problems, or even speech challenges.
The key thing to remember is that early evaluation is proactive. Addressing a functional restriction sooner prevents those deep-rooted compensation patterns from setting in, which are much harder to correct later on.
Is a Laser Frenectomy Painful for a Baby?
Your child’s comfort is our top priority, and we know this is a huge concern. A laser frenectomy is an incredibly quick and gentle procedure, often taking less than 60 seconds.
We use a strong topical numbing gel on the area first to make sure your baby is comfortable. The laser itself is a fantastic tool because it seals the nerve endings as it works, which dramatically minimizes discomfort both during and after the release.
Most babies get a little fussy—similar to how they might feel after vaccinations—but they can usually nurse or take a bottle right away. In fact, we encourage it! Feeding is a great comfort to them and immediately gets their newly freed tongue moving. The laser also means very little bleeding or swelling, making for a much smoother recovery.
What's the Difference Between a Tongue Tie and a Lip Tie?
This is a great question because these two issues often go hand-in-hand and can cause very similar problems with feeding.
- A tongue tie (ankyloglossia) restricts the tongue's movement. It’s that band of tissue underneath the tongue (the lingual frenulum) being too short or tight, keeping the tongue from lifting and moving like it should.
- A lip tie restricts the movement of the upper lip. The little band of tissue connecting the lip to the gum (the labial frenulum) is too tight, which stops the lip from flanging out for a good seal.
A tight lip tie can make it really tough for a baby to get a wide latch on a breast or bottle. This often leads to a shallow latch, clicking sounds, and swallowing a lot of extra air. Since the tongue and lip have to work together, a good evaluation will always check for both. Fixing one without the other might not solve the whole problem.
Why Is Therapy Needed After a Frenectomy?
Think of it this way: the frenectomy releases a muscle that has been tethered its whole life. It's never had a chance to learn how to move properly. Simply snipping the tie doesn't automatically teach the tongue what to do next.
This is where orofacial myofunctional therapy (OMT) comes in. It’s basically physical therapy for the tongue, mouth, and face. The goal is to retrain all those neuromuscular patterns for correct swallowing, breathing, and eventually, speech. For infants, this is usually guided by a lactation consultant or feeding therapist. Older kids will do specific exercises with an OMT to build strength and coordination.
Without this step, two things can happen. The tongue might never reach its full range of motion, or worse, the wound can heal back together and reattach, bringing the restriction right back. Therapy is absolutely essential to ensure the procedure delivers a successful, lasting improvement in your child's health and function.
At Pain and Sleep Therapy Center, we believe in looking at the whole picture to find the root cause of your child's challenges. From in-depth evaluations and gentle laser frenectomies to the crucial follow-up therapy, our team is here to support your family every step of the way. If you have concerns about your child's feeding, speech, or breathing, schedule a consultation with our experts today.