When you’re stuck searching for a "facial pain specialist near me," it’s usually because the pain itself has become unbearable. It's the kind of discomfort that completely derail your life—it messes with your sleep, makes it hard to focus at work, and can leave you feeling hopeless without any real answers.
The right expert won't just look at where it hurts. They'll dig deeper to find out why it hurts, whether the problem is coming from your jaw, your nerves, or even how you breathe at night.
Your Search for a Facial Pain Specialist Starts Here
Facial pain is way more than an inconvenience; it’s a complex signal from your body that something is off-balance. Because your face is packed with a dense network of nerves, muscles, and joints, figuring out the source isn't always straightforward. A lot of people first assume it's a sinus infection or a toothache, only to find the real culprit is something else entirely.
Think of this guide as your roadmap to finding genuine, lasting relief—not just masking the symptoms. We'll pull back the curtain on the interconnected world of orofacial pain and show you how issues that seem totally unrelated are often linked.
Understanding the Big Picture
A true facial pain specialist knows that your jaw (TMJ), nerves, muscles, and even your airway all work together as one system. When one part is out of sync, it can easily create a ripple effect of pain somewhere else.
This is exactly why a one-size-fits-all approach almost never works. The only way to get lasting results is with a treatment plan built on an accurate, comprehensive diagnosis.
This guide will walk you through:
- The Root Causes: We’ll break down the most common culprits behind facial pain, from TMJ disorders to nerve-related conditions.
- The Specialist's Role: You'll learn what to expect during a thorough evaluation and why it’s the most important step.
- Modern Treatment Options: We'll explore evidence-based therapies that go way beyond temporary fixes.
- Choosing the Right Expert: Get practical tips for finding a provider you can trust to guide you back to feeling normal.
Finding the right specialist is the most critical first step toward reclaiming your quality of life. An expert diagnosis from a dedicated team ensures your treatment targets the actual problem, not just the pain it causes.
Starting this journey can feel overwhelming, but you're not in it alone. By understanding the fundamentals of orofacial pain, you’ll be empowered to make informed decisions and find the expert care you deserve. To learn more about our dedicated team, you can meet our providers who specialize in this complex field.
Understanding What Causes Facial Pain
Facial pain is more than just a surface-level problem; it’s a complex signal that something deeper is out of balance. Because the face is such a dense hub of nerves, muscles, blood vessels, and joints all working in harmony, pinpointing the true source of your discomfort really requires a specialist's eye.
Think of it like a detective story. The pain is a clue, but it doesn't always point directly to the offender. The real cause might be mechanical, neurological, or even referred from another part of your body entirely. Getting to the bottom of it is the first real step toward finding relief.
Temporomandibular Joint (TMJ) Disorders
One of the most frequent culprits behind facial pain is the temporomandibular joint, or TMJ. This is the intricate, sliding hinge that connects your jawbone to your skull. When it functions correctly, you can talk, chew, and yawn without giving it a second thought.
But when this complex system of muscles, ligaments, and bone gets strained or misaligned, it can lead to a TMJ disorder (TMD). This dysfunction can trigger a whole host of symptoms, from a dull, persistent ache in your jaw to sharp pains that radiate to your ear, temple, or neck. Some people hear clicking or popping sounds, while others find their jaw locks up or can barely open.
To see if these signs sound familiar, you can check out our detailed guide on the symptoms of temporomandibular joint dysfunction.
Neuropathic and Referred Pain
Sometimes, the pain has nothing to do with a joint or muscle at all. Instead, it originates from the nerves themselves. This is known as neuropathic pain, and it often feels very different from a typical ache.
Neuropathic facial pain is often described as a sudden, sharp, or electric shock-like sensation. It happens when nerves misfire and send faulty pain signals to the brain, even when there's no actual injury where you feel the pain.
Trigeminal neuralgia is a classic example, causing intense, stabbing pain on one side of the face.
Then there’s referred pain, which is when your brain gets its wires crossed. A problem in one area, like a tense muscle in your neck or shoulder, can send pain signals that show up in your jaw or cheek. Your face hurts, but the actual problem is somewhere else entirely. This is exactly why a thorough examination of the entire head and neck system is so critical.
Facial pain isn't a rare issue. Research shows that approximately 3.4% of the population experiences frequent pain in their temple, face, or jaw. This growing awareness is even reflected in search trends, which have seen a huge increase in people looking for specialized care. You can read the full research about these trends and statistics.
What to Expect During Your First Specialist Visit
Walking into any new doctor's office can feel a little unnerving, especially when you've been living with chronic pain. But a visit to a facial pain specialist is completely different from your typical medical check-up. The first consultation isn't about just managing symptoms; it’s a deep dive designed to uncover the real reason behind your discomfort.
Think of it as a detailed investigation. We’ll start with a comprehensive conversation about your medical history, but we go much deeper than just the basics. I’ll want to know everything about your pain: when it started, what it feels like, what makes it better or worse, and how it’s affecting your daily life—including your sleep and stress levels.
This in-depth discussion helps me connect the dots and see the bigger picture, often revealing clues that were missed before.
The Comprehensive Physical Evaluation
After our talk, I’ll conduct a thorough, hands-on examination. This is a critical step that goes way beyond just looking at the area that hurts. I'll be carefully assessing a few key things:
- Your Head and Neck: I’ll evaluate the muscles for hidden tension, trigger points, and imbalances that could be referring pain straight to your face.
- Your Jaw (TMJ): I’ll check its range of motion, listen for any clicking or popping sounds, and feel exactly how the joint moves.
- Your Bite and Teeth: I'll observe how your teeth fit together. Even a slight misalignment can put a tremendous amount of strain on your jaw joints and facial muscles.
- Your Posture and Breathing: I’ll even assess how you hold your head and shoulders and observe your breathing patterns, as these habits directly influence facial muscle strain.
This hands-on approach provides invaluable information about the structural and functional issues contributing to your pain. It tells a much richer story than symptoms alone ever could.
A top-tier facial pain specialist acts like a detective, using every piece of information—from your sleep quality to your posture—to build a complete case file. This ensures the final diagnosis is accurate and the treatment plan is targeted precisely at the source of the problem.
Advanced Diagnostic Tools
To complete the picture, we often use advanced diagnostic technology to look beneath the surface. While every clinic is different, this usually includes 3D Cone Beam Computed Tomography (CBCT) imaging. This incredible tool gives us a detailed, three-dimensional view of your jaw, airway, and facial structures, allowing us to see problems that standard X-rays would completely miss.
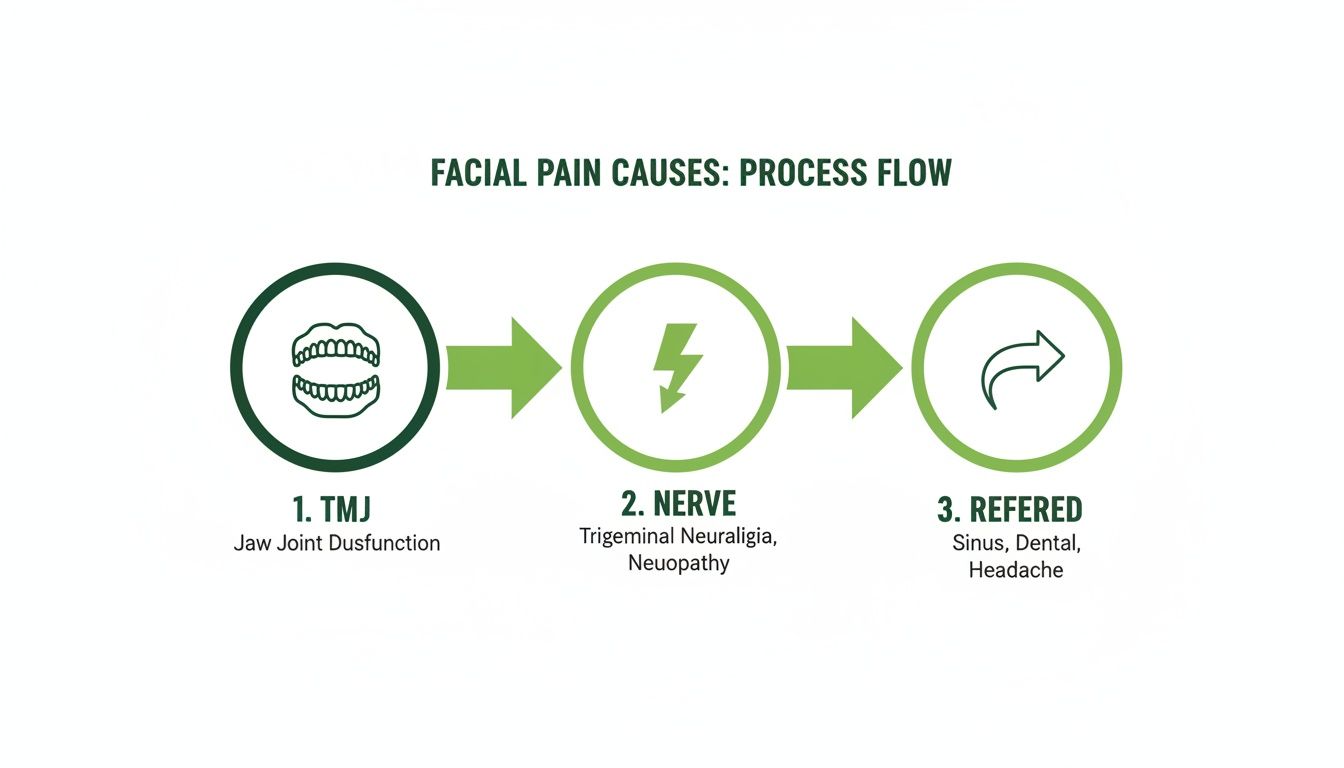
This infographic shows how different sources of pain—like TMJ disorders, nerve issues, or referred pain—can be identified through this process.
By combining your story, a physical exam, and precise imaging, we can finally get to the bottom of what's going on. It’s this multi-faceted approach that allows us to confidently identify the true cause of your pain and create an effective, personalized treatment plan to bring you lasting relief.
Exploring Modern Treatments Beyond Pills and Surgery

If you've been dealing with chronic facial pain, it’s easy to feel like your only options are a life sentence of pain medication or invasive surgery. But the world of orofacial pain management has come a long way from just masking symptoms.
Today’s specialists have shifted focus to restorative, non-invasive therapies that work with your body. The goal isn’t just to quiet the pain—it’s to heal the underlying tissue damage, muscle dysfunction, or airway issues that are actually causing it. This approach offers a path to genuine, long-term relief.
Harnessing Your Body’s Healing Power
One of the most exciting advancements is in regenerative therapies. Instead of relying on foreign substances, these treatments use your own body’s biological building blocks to repair and rebuild damaged tissues in and around your jaw joint.
Think of it like giving a construction crew the highest-quality materials to fix a crumbling foundation. These therapies provide your body with the exact resources it needs to heal itself from the inside out.
Two of the leading regenerative options include:
- Prolotherapy: This involves injecting a natural solution, often a dextrose compound, into ligaments or tendons that have become weak. This creates a mild, controlled inflammation that jump-starts your body’s natural healing process, encouraging it to build new, stronger tissue to stabilize the joint.
- Platelet-Rich Fibrin (PRF): This therapy uses a concentrate of platelets and growth factors taken from a small sample of your own blood. When injected, PRF acts like a natural scaffold that promotes cell regeneration, calms inflammation, and speeds up tissue repair.
These methods are changing the game for patients who previously had very few options. It’s part of a massive shift in pain management, a field projected to reach USD 106.86 billion by 2031, with facial pain and migraine care being some of the fastest-growing areas. You can see more details on this growth over at mordorintelligence.com.
Retraining Muscles and Restoring Function
Pain isn't just about what's happening in your joints and tissues; it's also deeply connected to function and habit. A truly forward-thinking facial pain specialist near me will dig deeper and look at how you use your facial muscles every single day.
Lasting relief often requires re-educating the very system that created the problem. This means correcting the subtle but powerful muscle functions, breathing patterns, and posture that contribute to chronic strain and pain.
This is where therapies focused on function come into play. Many modern specialists now incorporate a two-pronged approach that combines joint-focused treatments with therapies that retrain harmful muscle habits.
Comparing Modern Facial Pain Treatment Approaches
The table below breaks down the difference between older, symptom-based methods and the innovative, root-cause therapies we use today.
| Treatment Approach | Focus | Goal | Examples |
|---|---|---|---|
| Traditional Pain Management | Symptom Suppression | Temporarily reduce or mask pain signals. | Pain medication, muscle relaxers, corticosteroid injections. |
| Surgical Intervention | Structural Alteration | Physically alter the joint or surrounding structures. | Arthrocentesis, arthroscopy, open-joint surgery. |
| Modern Regenerative Therapy | Tissue Healing | Stimulate the body's own repair mechanisms. | Prolotherapy, Platelet-Rich Fibrin (PRF). |
| Functional Therapy | Root-Cause Correction | Retrain improper muscle function and habits. | Orofacial Myofunctional Therapy (OMT), airway/sleep therapy. |
As you can see, the modern approach is about creating sustainable, long-term health rather than just offering a temporary fix.
Orofacial Myofunctional Therapy (OMT) is essentially physical therapy for your face, tongue, and jaw. A trained therapist guides you through specific exercises designed to correct habits like improper breathing, chewing, and swallowing. OMT helps restore correct tongue posture and promotes nasal breathing, which takes a tremendous amount of strain off the TMJ and surrounding facial muscles.
In the same way, addressing sleep and airway issues is absolutely critical. Obstructed breathing at night can force your jaw into stressful positions for hours, leading to those familiar morning headaches and facial pain. By improving how you breathe, a specialist can dramatically reduce the nightly strain that keeps you stuck in a pain cycle. To explore this further, take a look at our guide on TMJ treatment options.
How to Choose the Right Facial Pain Specialist for You
Finding the right facial pain specialist is probably the single most important step you'll take toward getting your life back. Think of it less like finding a doctor and more like hiring a detective for a really complex case—your own. You need someone who can connect all the clues, not just patch up the symptoms.
A great specialist knows your pain isn't just in your jaw. They understand how your bite, the way you breathe, your posture, and even how you sleep are all tangled together. Making the right choice means finding a professional who is genuinely committed to digging deep and figuring out that bigger picture.
Credentials and Specialized Training
First things first, check their credentials. While plenty of healthcare professionals can treat pain, orofacial pain is its own distinct specialty. You’ll want to look for a provider who is board-certified in Orofacial Pain. This certification is the gold standard and signals they’ve reached the highest level of expertise in this field.
But don't stop there. Dig into their specific training. A truly comprehensive approach requires a unique blend of skills, including:
- Dental Sleep Medicine: This is a huge one. It’s critical for linking facial pain back to hidden sleep and airway problems.
- Neuromuscular Dentistry: This expertise focuses on the delicate relationship between your jaw muscles, nerves, and bite.
- Regenerative Therapies: This tells you they’re using modern treatments that help your body actually heal itself, not just mask the pain.
A specialist with this kind of background can see your condition from every angle, making sure no stone is left unturned.
A Focus on Diagnostics and Technology
You wouldn't want a mechanic to start taking apart your engine without running a full diagnostic scan first, right? The same logic applies here. The best clinics invest in advanced tools to get a crystal-clear picture of what's really going on beneath the surface.
A specialist's commitment to technology is a direct reflection of their commitment to an accurate diagnosis. Tools like 3D Cone Beam Computed Tomography (CBCT) are essential for visualizing the jaw joints, airway, and facial structures in detail, revealing issues that standard X-rays would miss entirely.
When you call a potential office, just ask them what kind of diagnostic equipment they use. Their answer will speak volumes about how seriously they take getting to the root of the problem.
Reading Between the Lines of Patient Experiences
Finally, look beyond the clinic’s polished website and read what actual patients are saying. Don't just scan the star ratings; dive into the details of their reviews and testimonials.
Do people mention feeling truly heard and understood? Do they talk about how the specialist took the time to explain everything, making them a partner in their own care? These personal stories give you invaluable insight into a provider’s communication style and patient-first philosophy. It's the best way to find a facial pain specialist near me who is not only qualified but who will also be a true ally in your recovery.
Your Questions About Facial Pain, Answered
When you’re dealing with persistent facial pain, a lot of questions come up. It's completely normal to feel uncertain, and finding clear answers is the first step toward getting help.
We hear these same questions from patients every day. So, let’s walk through some of the most common ones to give you the clarity you need to move forward.
How Can I Tell If My Pain Is From TMJ or My Sinuses?
This is easily one of the biggest points of confusion we see. The symptoms—pressure, aching around the cheeks, even pain behind the eyes—can feel almost identical.
The trick is to look for clues that point to one or the other.
Sinus pain usually comes with a few tell-tale signs:
- Nasal congestion or a stuffy, blocked feeling
- Thick, colored nasal discharge
- A dulled sense of smell
- Pain that gets noticeably worse when you bend forward
On the other hand, TMJ-related pain is almost always tied to jaw function. Does the pain flare up when you chew, talk, or yawn? That’s a big clue. Other classic signs of a TMJ disorder include clicking or popping sounds in your jaw, tenderness right in front of your ears, or a feeling that you can't open your mouth all the way. While a stuffy nose makes sinusitis the obvious suspect, studies often show that a thorough evaluation points to a different cause altogether.
Does All Facial Pain Come From ENT or Dental Issues?
Not at all, and this is a critical point. While a sinus infection or a bad tooth are definitely common culprits, the source of facial pain is often neurological or musculoskeletal.
Take a condition like trigeminal neuralgia, for example. This comes from the nerves themselves, causing sharp, electric-shock sensations that have absolutely nothing to do with your teeth or sinuses. We also see pain referred from tight muscles in the neck and shoulders, which can show up as a dull ache in the jaw or face. This is exactly why a specialist with a deep understanding of the entire head and neck system is so vital for getting an accurate diagnosis.
It's a common myth that all facial pain has a structural cause you can spot on a simple X-ray. The truth is, many conditions are functional or neurological, requiring a much deeper diagnostic look to find the real source of the problem.
What Happens If I Just Ignore My Facial Pain?
Ignoring persistent facial pain almost always leads to a steady decline in your quality of life. Think about it—chronic discomfort messes with your sleep, makes it hard to focus at work, and can turn simple things like eating a meal into a painful ordeal.
Beyond the day-to-day impact, letting the root cause go untreated allows it to get worse. An unaddressed TMJ disorder, for instance, can lead to more significant joint damage over time. If an infection is behind the pain, it could spread and cause far more serious complications. The best thing you can do is get a professional evaluation to figure out what's going on and stop it from becoming a bigger problem down the road.
How Quickly Can I Expect Relief?
This really depends on what’s causing the pain in the first place.
If it's an acute bacterial sinus infection, you might feel a world of difference within a few days of starting antibiotics. But for chronic conditions like TMJ disorders or neuropathic pain, the path to relief looks different. It often involves a more thoughtful, long-term management plan.
Regenerative therapies and Orofacial Myofunctional Therapy, for instance, don't just mask the pain—they work to heal tissues and correct the underlying habits. The improvement is usually gradual, but it’s real and sustainable. Our goal isn’t a quick fix; it’s lasting recovery.
At the Pain and Sleep Therapy Center, we specialize in providing the answers and effective treatments you've been looking for. If you're ready to move beyond the uncertainty and find a clear path to relief, we invite you to schedule a consultation with our dedicated team. Learn more and book your visit at https://pscharlotte.com.